
B
arbosa
DC
et
al
.
358
R
ev
A
ssoc
M
ed
B
ras
2017; 63(4):355-360
eral enzymatic and non-enzymatic buffering systems, with
anti-inflammatory and analgesic action.
31-33
Ozone’s mechanism of action in the treatment of
FBSS is little known. Current hypotheses suggest that its
effect could occur through chemical adhesiolysis of scar
fibrosis associated with pain and dehydration of the her-
niated disc contents,
31
as well as the activation of cytokines
that would inhibit proinflammatory factors associated
with chronic pain.
32
It is believed that ozone may cause
local vasodilation, favoring the neutralization of acidosis
and the induction of antioxidant enzymes associated with
analgesia, as well as stimulating the activation of the
descending antinociceptive system, blocking the transmis-
sion of pain to the thalamus and cortex.
33
Interest in the effects of ozone therapy to treat FBSS
has been growing in the last two decades. Intradiscal
and paravertebral ozone injection associated with a ste-
roid and local anesthetics have presented significant
results. Gallucci et al.
34
compared the effect of adding
ozone to a mixture of steroid and anesthetic in 159 pa-
tients. They reported that the ozone-treated group showed
more improvement than the patients who did not receive
it within six months of follow-up. In addition to the role
of ozone in FBSS, Bonetti et al.
35
suggest that its anal-
gesic action is also reproducible in chronic LBP and lum-
bago with sciatica.
When evaluating the intraforaminal effect of ozone
versus steroidal infiltration in 306 patients, the authors
observed that those treated with the oxygen-ozone mixture
showed more improvement than the group treated with
corticosteroids alone. In a meta-analysis by Magalhães et
al.,
29
the level of evidence attributed to long-term pain
relief was II-3 in the case of intradiscal ozone and II-1 for
paravertebral ozone. Although the evidence corroborates
the efficacy of intradiscal and paravertebral ozone injec-
tion, there is still little data on epiduroscopy-assisted use.
In a pilot study with 13 patients published by Magalhães
et al.,
28
the effect of the ozone-oxygen mixture versus
oxygen in the epidural space was compared after adhe-
siolysis. Patients with PNNP presented a significant reduc-
tion in pain and disability according to ODI, whereas in
the PNP group this reduction was not significant, which
TABLE 2
Mean of results obtained from the scales applied before and 21 days after the procedure (n=19).
Scales
Pre-surgery*
21 days*
p**
Visual Analogue Scale (VAS)
8.47 (± 1.12)
7.05 (± 2.68)
0.029
Neuropathic Pain Symptom Inventory (NPSI)
62.74 (± 20.99)
54.21 (± 28.50)
0.034
Oswestry Disability Index (ODI)
37.58 (± 5.58)
35.84 (± 7.62)
0.217
Roland-Morris Disability Questionnaire
14.47 (± 5.08)
13.84 (± 6.32)
0.438
Brief Pain Inventory (BPI)
Intensity
7.86 (± 1.11)
6.58 (± 2.15)
0.005
Interference
7.63 (± 1.54)
6.71 (± 2.45)
0.054
*Scale values expressed as mean and standard deviation; **Student’s paired t-test.
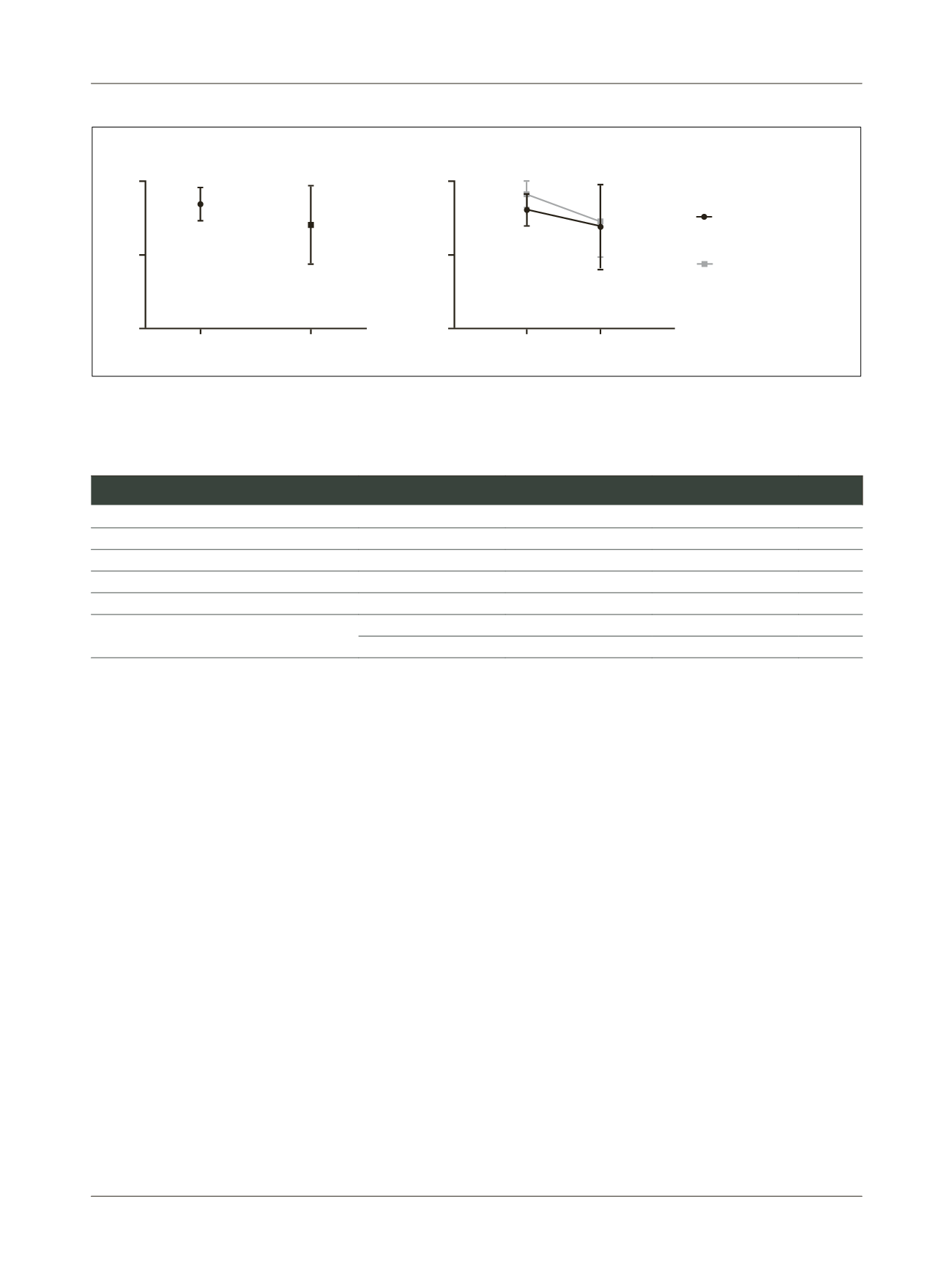
A
B
Pre
10
10
5
5
0
0
Pre
Post
Post
V
A
S
V
A
S
Predominantly
neuropathic pain
Predominantly
non-neuropathic pain
FIGURE 1
A. Statistical analysis of VAS after epiduroscopy with ozone injection, evidencing a significant reduction in scores (Student’s paired
t-test with p<0.05). B. Comparison of VAS in patients with PNP and PNNP pain (Repeated Measures ANOVA with p>0.05).
















