S
tevens
-J
ohnson
syndrome
and
toxic
epidermal
necrolysis
:
a
review
R
ev
A
ssoc
M
ed
B
ras
2016; 62(5):468-473
471
good history, with emphasis on the use of drugs and the
occurrence of previous infections, and thorough physi-
cal examination are essential.
Drug provocation tests are contraindicated, since a
subsequent exposure to the agent could trigger a new se-
vere episode of SJS/TEN.
13
Complete blood count (CBC) may show unspecific
leukocytosis or even indicate superimposed secondary
bacterial infection. Cultures of blood, urine and skin may
reveal the agent of the underlying suspected infection.
13
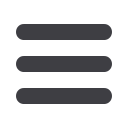
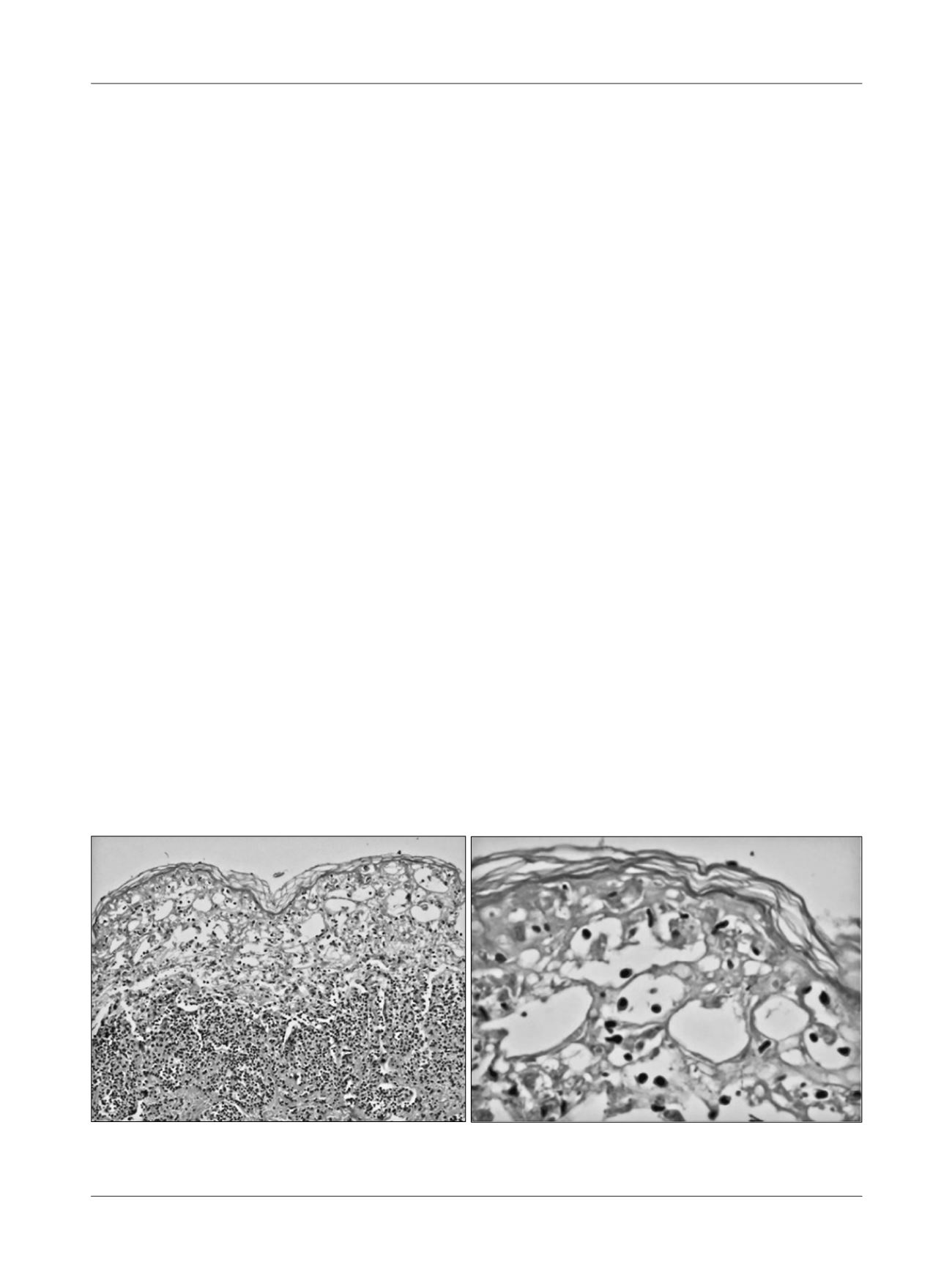
Skin biopsy is an additional final examination and
reveals necrosis in all layers of the epidermis caused by
apoptosis of keratinocytes and epidermal detachment,
while the dermis displays minimum inflammatory chang-
es
1
(Figure 2).
Serum levels of tumor necrosis factor-alpha and sol-
uble Il-2, Il-6 and C-reactive protein receptors are typi-
cally elevated in patients with SJS, although none of
these serological tests are used routinely for diagnosis
in our midst.
D
ifferential
diagnosis
The most important differential diagnoses include dis-
orders involving the peeling of the skin, such as erythe-
ma multiforme major, herpes simplex virus (HSV)–asso-
ciated erythema multiforme, burns, widespread fixed drug
eruption, acute generalized exanthematous pustulosis,
erythroderma, bullous pemphigoid, linear IgA dermato-
sis, paraneoplastic pemphigus, lymphoma, angioimmu-
noblastic lymphadenopathy, viral rashes, secondary syph-
ilis, herpetic gingivostomatitis, staphylococcal scalded
skin syndrome, graft
versus
host disease and autoimmune
vasculitis.
1-3,13
T
reatment
Management of patients with SJS or TEN requires three
measures: removal of the offending drug, particularly
drugs known to be high-risk; supportive measures and
active interventions.
Early diagnosis of the disease, recognition of the caus-
al agent and the immediate withdrawal of the drug are
the most important actions, as the course of the disease
is often rapid and fatal.
Figuring out the offending drug may not be easy and,
in these cases, all drugs non-essential to the maintenance
of the patient’s life should be suspended.
S
upport
treatment
Patients should preferably be treated in burn units. The
first care should include supportive and symptomatic
measures: body temperature control, hydration and elec-
trolyte replacement, special attention to the airways, pre-
venting secondary infection, pain control, maintenance
of venous access distant from the affected areas, early oral
nutrition or parenteral nutrition, if necessary, and anti-
coagulation.
7,14
Skin lesions are treated according to the protocol for
patients with large burns. There is no consensus on top-
ical care. Topical antiseptics can be used, or just soap and
water, in quick baths.
7
The practice of debridement is controversial.
Prophylactic antibiotic therapy is not recommended
as it can induce resistance and because these drugs can
per se
be causative agents of SJS or TEN. Therefore, they
are given only in proven cases of infection, or when there
is sudden decrease/rise in temperature, poor general con-
dition, or positive skin cultures.
14
FIGURE 2
Pathological examination of the skin of a patient with Stevens-Johnson syndrome.















