B
reast
cancer
:
news
in
diagnosis
and
treatment
R
ev
A
ssoc
M
ed
B
ras
2015; 61(6):543-552
547
histology and immunohistochemical markers. Moreover,
the fragments removed are larger (in size and number),
there is less mobilization of breast tissue, and the device
is introduced once only, providing greater comfort to the
patient, and also being more convenient for the physi-
cian. Finally, it allows pre-operative treatment planning.
Disadvantages include discomfort that puncturing can
produce in anxious patients and particularly the meth-
od’s high cost.
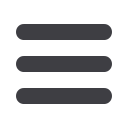
Preoperative marking consists of preoperative loca-
tion of suspected non palpable breast lesions. Can be made
with a harpoon-shaped guide wire (“needling”) (Figure 4)
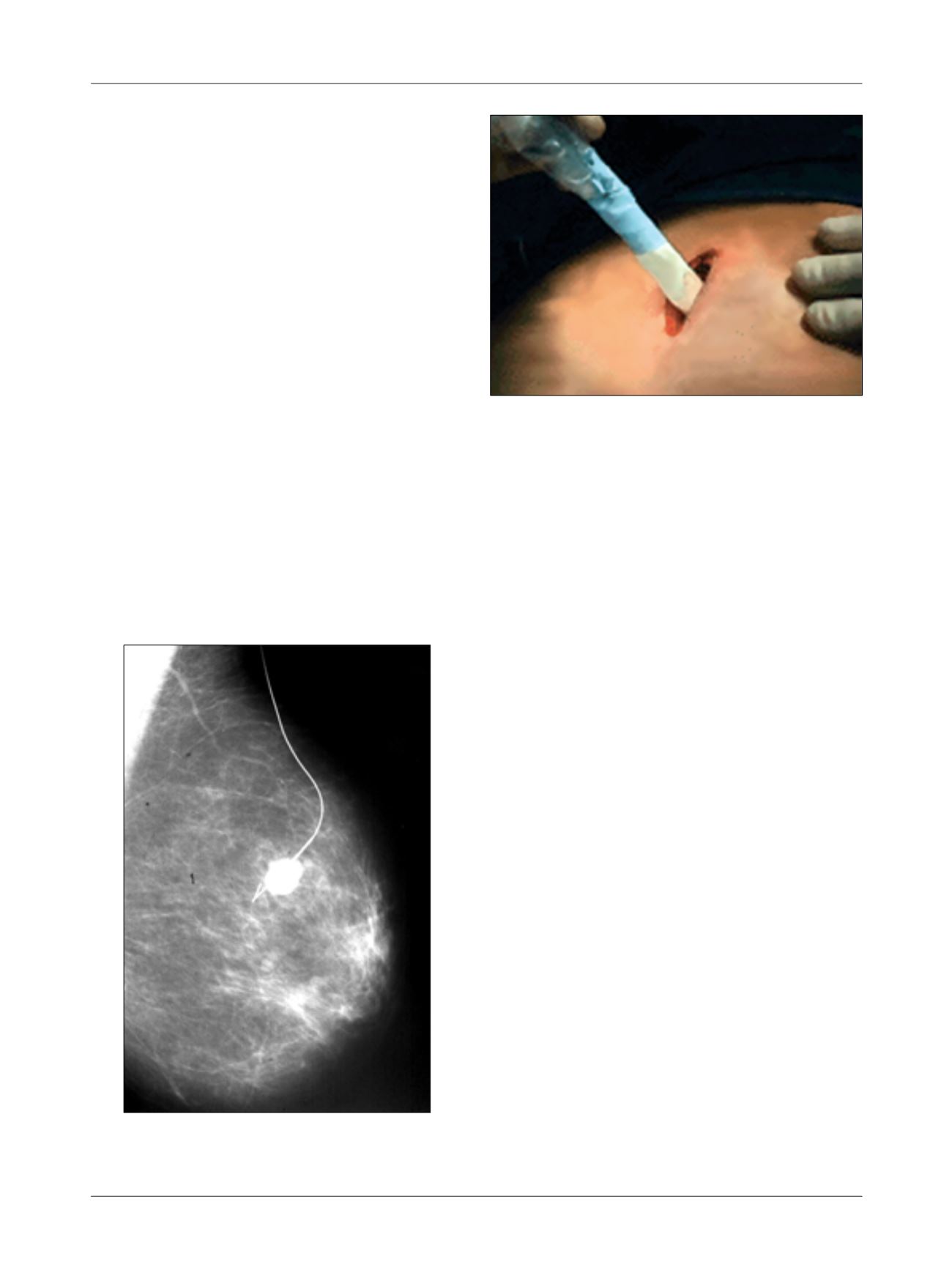
or by injection of a radioactive substance, a technique
known as ROLL (radioguided occult lesion localization)
(Figure 5). In both cases, marking can be performed us-
ing stereotactic mammogram or ultrasound.
When using stereotactic mammogram, the harpoon
inserted before surgery should be placed 1.0 cm after the
lesion, which allows it, even if the repair shifts, to contin-
ue to be close enough to the biopsy area. In ROLL, the scin-
tigraphic emission is detected on the skin surface by gam-
ma detector probe intraoperatively
.
It is more accurate and
less invasive, but requires assistance of the nuclear medi-
cine team and the cost is higher. In suspected calcifications,
mammogram of the surgical specimen is essential to con-
firm the removal of the previously marked lesion.
Preoperative marking has an advantage compared to
methods of percutaneous biopsy, which is the fact that
the material is abundant for pathological study, allowing
better diagnostic definition and proper assessment of the
resection margins. The main disadvantages are the need
for hospitalization, anesthesia, a larger surgical scar, and
the possibility of changes in subsequent images on mam-
mogram and/or ultrasound. Furthermore, BI-RADS IV
lesions are benign in 80% of cases on average, i.e., surgery
is actually required in 20% of cases. The failure rate in re-
moval ranges from 0.2 to 22%, with an average of 4%.
Once a diagnosis of breast cancer is made, it must be
staged. The clinical stage of breast cancer is based on the
TNM classification (T = tumor size; N = axillary lymph
nodes; M = distant metastases). Staging is both clinical
(cTNM) and pathologic (pTNM).
T
reatment
Halsted, in the late nineteenth century, proposed that
breast cancer was a local disease, spreading it in an order-
ly and centrifugal manner to the axillary lymph nodes,
which would act as an actual barrier to the spread of dis-
ease. Hence, the importance of resection of the breast and
lymph nodes in the most radical way possible, to eradi-
cate disease and improve survival. Highly radical surgi-
cal and radiotherapy prevailed in the first half of the twen-
tieth century, but soon began to show disappointing
results, because patients with small tumors treated in
such an aggressive way would succumb, paradoxically, in
relatively short times.
FIGURE 4
Preoperative marking with metallic harpoon – needling.
FIGURE 5
Intraoperative localization with gamma ray detection
probe – ROLL.















