N
azário
ACP
et
al
.
546
R
ev
A
ssoc
M
ed
B
ras
2015; 61(6):543-552
cer is unknown. It is indicated when the extent of the sus-
pected lesion cannot be determined by conventional meth-
ods, such as in dense breast tissue or when the diagnosis
is lobular carcinoma; in women at high risk for develop-
ing breast cancer, such as the carriers of
BRCA1
and
BRCA2
gene mutations; to monitor the response to neoadjuvant
chemotherapy; to assess the integrity of the prosthesis
and in diagnoses of presumed occult breast carcinoma
(i.e., presence of metastasis in the axilla without evidence
of primary disease on clinical examination, mammogram
and ultrasound).
Recently, tomosynthesis or 3D mammogram was in-
troduced, with the promise to detect more lesions than
digital mammography. However, its use as a routine did
not prove to decrease mortality.
The American Cancer Society of Breast Diseases rec-
ommends that mammogram screening starts at the age
of 40 years, being annual from this age. The Brazilian
Ministry of Health, in turn, recommends that women at
low risk for developing breast cancer undergo bi-annual
mammograms, beginning at the age of 50. In the case of
high-risk women, the ministry advises that the examina-
tion should be carried out annually from the age of 35,
or 10 years before the age of diagnosis of the youngest af-
fected relative. The Brazilian Society of Mastology sug-
gests that mammogram is made annually between 40 and
49 years, and biannually thereafter. In 2015, the Ameri-
can Cancer Society began recommending that mammo-
gram should be done annually between 45 and 54 years,
and every two years thereafter. In São Paulo, the propor-
tion of cases between 40 and 49 years (21.3%) is very close
to that found between 50 and 59 years (27%). Thus, we
recommend annual mammogram from the age of 40 years,
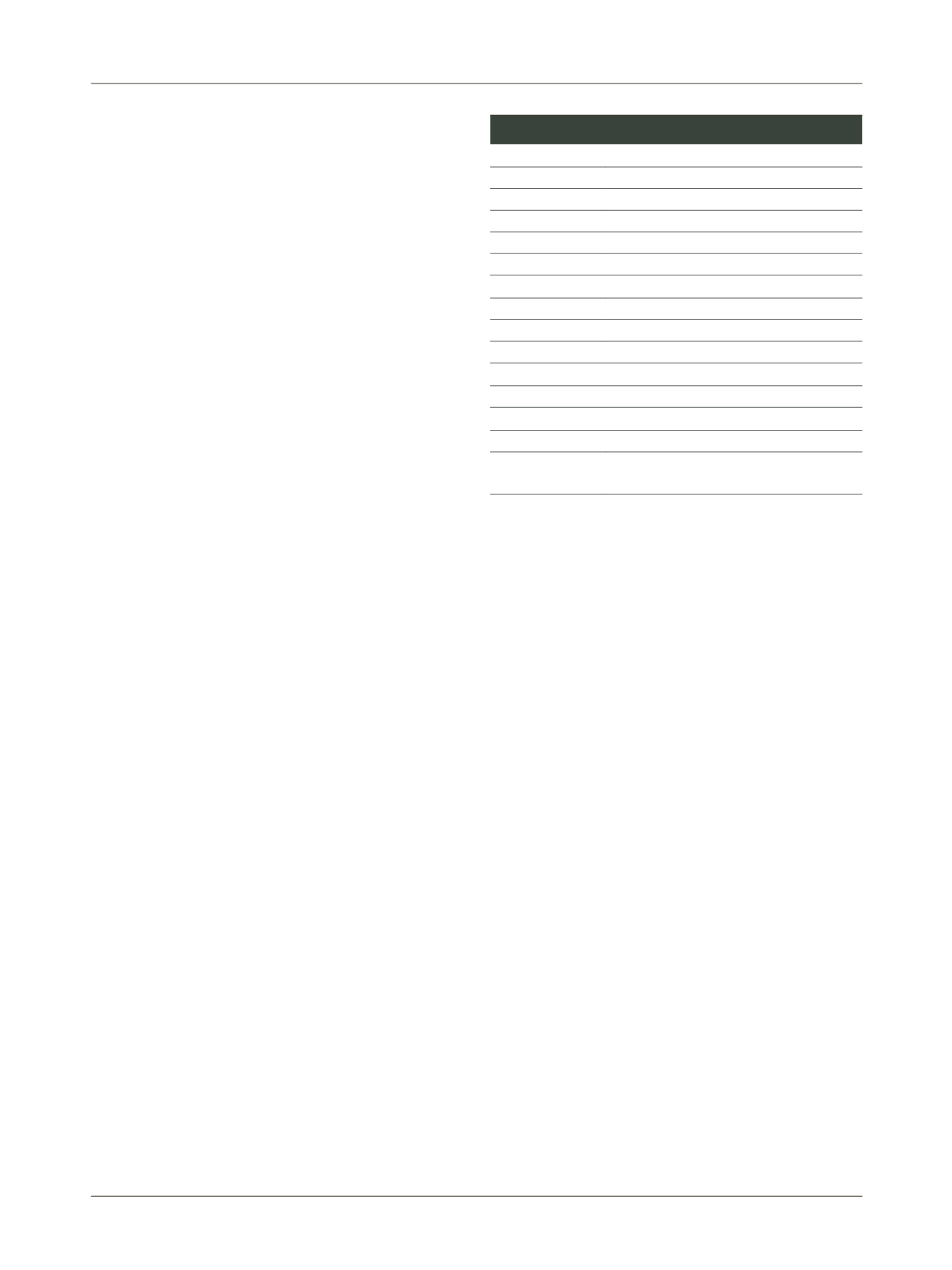
ending when life expectancy is less than five years. Table
2 summarizes the various guidelines.
In cases of suggestive lesions, percutaneous biopsies
are preferred. The first is biopsy with fine needle (FNAB),
an outpatient method with low cost and relatively sim-
ple
.
The needle (25/6
gauge
) makes the procedure com-
fortable and virtually risk-free. It can be done by palpa-
tion, but preferably ultrasound-guided, due to a higher
predictive value. FNAB is contraindicated for investiga-
tion of suspected calcifications. Its disadvantages include
the impossibility of evaluating invasion and histological
grade. Moreover, it is very difficult to determine the his-
tological type and the expression of hormone receptors.
The false positive rate is very low (between 0 and 2%). How-
ever, 5-20% of cases are false negatives, mainly due to im-
proper technique for slide preparation. Thus, in cases of
suspected image but negative, unsatisfactory or inconsis-
tent FNAB compared to the clinical-imaging diagnosis,
investigation should continue.
Core needle biopsy (CNB) is done with a large needle
and an automated device that propels and retracts the nee-
dle that cuts the tissue. It is indicated for suggestive nod-
ules larger than 1.0 cm or extensive calcifications. Under
those conditions, sensitivity is 48 to 100% and specificity,
91 to 100%. On the other hand, it is contraindicated in case
of deep image alterations (risk of pneumothorax and he-
mothorax), fibro-glandular distortion, in suggestive asym-
metries, patients with hypomastia, or lesions adjacent to
breast implant.
Advantages include the fact that it is an outpatient
method, requiring local anesthesia. It allows evaluation
of invasion, histological type and immunohistochemical
expression, and the definition of a preoperative treatment
planning. Cost (moderate), fragmentation of the materi-
al, and the mobilization of the breast tissue simulating
invasion and/or embolization are the disadvantages. Anx-
ious patients may find the procedure uncomfortable.
Mammotomy with core needle biopsy (CNB) is per-
formed using a vacuum system with hollow
cannula
, which
rotates at high speed, cutting through the tissue that is
sucked out of the breast. It is also known as vacuum-as-
sisted CNB
.
It is especially indicated for nodules smaller
than 1.0 cm, unpronounced suspected calcifications, fi-
bro-glandular distortion and asymmetric densities. Sen-
sitivity reaches 93% and specificity, 98%.
As in the case of core biopsy, mammotomy has the
advantage of being an outpatient method, using only lo-
cal anesthetics. It makes it possible to evaluate invasion,
TABLE 2
Early detection and screening for breast cancer.
Brazilian Ministry of Health (2004)
Group without risk 40 – 49 years: Annual physical exam
50 – 69 years: Annual physical exam
Mammogram every two years
High-risk group
From the age of 35 years: Annual physical exam
Annual mammograms
Brazilian Society of Mastology (2002)
40 – 49 years: Annual mammograms
50 – 69 years: Mammogram every two years
≥ 70 years: Depending on life expectancy
American Society of Breast Diseases (2006)
From the age of 40 years: Annual mammograms
American Cancer Society (2015)
45 – 54 years: Annual mammograms
After 55 years: Mammogram every two years (provided that life
expectancy is greater than 10 years)















