A
pproach
to
concurrent
coronary
and
carotid
artery
disease
: E
pidemiology
,
screening
and
treatment
R
ev
A
ssoc
M
ed
B
ras
2017; 63(11):1012-1016
1015
taneous carotid stenosis did not reduce the risk of CVA
in patients undergoing CABG, except for the subgroup
of symptomatic patients (CVA/TIA) with bilateral ca-
rotid obstruction, in whom hybrid staged treatment could
present a better neurological outcome in centers experi-
enced and qualified for such procedure.
19
Comparing CABG alone versus PCI + CABG (11) per-
formed within a mean interval of 5-6 weeks, there is a trend
in absolute numbers of higher risk of death, CVA and AMI
with combined surgery, respectively 0.9, 3.6 and 1.8% vs.
3.2, 6.4 and 6.4%, but without statistical significance. We
emphasize that this study was performed by a medical
center with extensive experience in carotid angioplasty and
should be taken into account when observing the results.
The lack of standardization of current studies, for
instance the surgical technique (percutaneous interven-
tion versus endarterectomy with or without a filter basket),
demographic and symptomatic profile of patients, and a
small number of patients, often without randomization,
make comparisons and broad definition of the best ap-
proach difficult. A feasible percentage, which would func-
tion as a treatment target, would be < 3% in the rate of
complications following carotid angioplasty in asymp-
tomatic patients, and < 6% in symptomatic patients.
10,25
C
onclusion
As already mentioned, the association of carotid and
coronary atherosclerosis is very prevalent, with no con-
sensus to date on which sequence of surgical approaches
is the safest. In fact, greater importance should be given to
intraoperative care, focusing on strict control of systemic
blood pressure, avoiding extreme BP levels and including
careful evaluation of the aorta during clamping and can-
nulation, as well as monitoring of cerebral oxygenation.
2
The risks inherent to the procedure should be considered
(higher CVA rate in revascularization surgeries in the pres-
ence of carotid disease and higher rate of AMI in carotid
surgeries concomitant with significant CAD) in the thera-
peutic decision (Figure 1). Individualization of treatment,
use of less invasive techniques (PCI whenever possible or
endovascular treatment of carotid arteries), and shared
decisions with the Heart Team should be encouraged.
Surely the maxim that advocates treatment of the most
severe entity in the first place has a place in this scenario.
C
onflict
of
interest
The authors declare no conflict of interest.
R
esumo
Abordagem da doença coronariana e carotídea concomi-
tante: epidemiologia, rastreamento e tratamento
A concomitância entre doença arterial coronária e doença
carotídea é conhecida e já bem documentada. Fato é, porém,
que, a despeito dos métodos de rastreio dessas condições
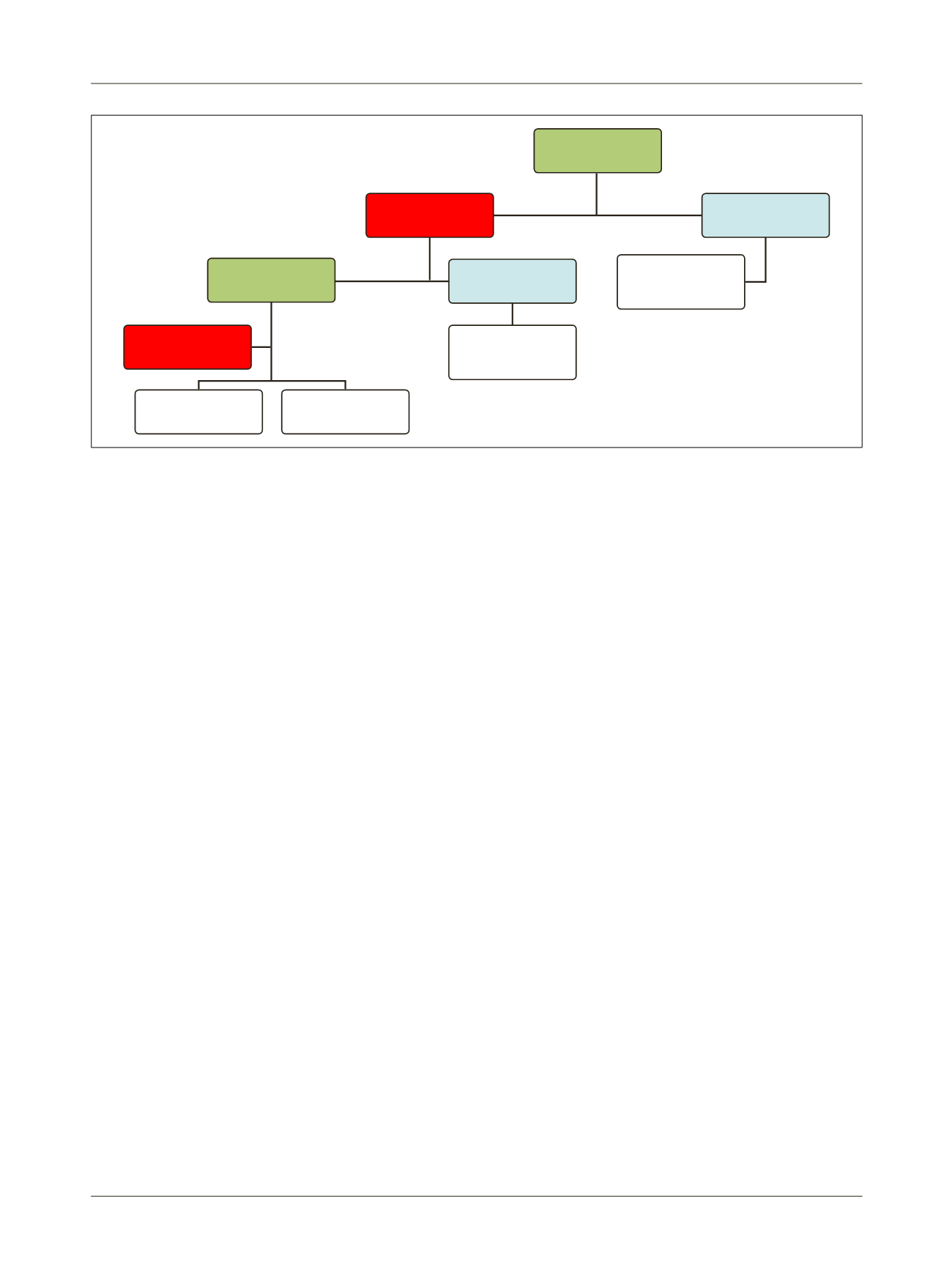
FIGURE 1
Suggested algorithm for therapeutic management of concurrent carotid and coronary artery disease.
CABG: surgical myocardial revascularization; CAR: carotid artery revascularization surgery.
High neurological risk: Clinical variables: symptomatic patient (previous stroke or TIA, amaurosis fugax, ischemic or infarction areas in CNS images, even without previous neurological symptoms).
Angiographic variables: bilateral carotid stenosis 70-99%, unilateral carotid stenosis 70-99% + contralateral occlusion.
High cardiac risk, clinical variables: unstable angina, CCS III-IV angina, acute coronary syndrome (AMI, STEMI or non-STEMI). Angiographic variables: left coronary artery lesion greater than 70%,
or proximal anterior descending (AD) artery greater than 90%, or AD and proximal circumflex (CX) > 70%, one of them greater than 90%.
High
neurological risk?
Simultaneous
CABG + CAR
Hybrid treatment
Carotid approach
(at the vascular
surgeon’s discretion)
Coronary approach
(at the cardiac
surgeon’s discretion)
Yes
No
Yes
High cardiac risk?
No
















