W
hat
is
the
role
of
routine
ultrasonography
performed
in
the
first
trimester
of
low
-
risk
pregnancy
?
R
ev
A
ssoc
M
ed
B
ras
2017; 63(1):4-6
5
ing the exact date of the last menstrual period or the
misinterpretation of genital bleeding related to egg im-
plantation as menstrual bleeding. In addition, the conven-
tion of a 14-day interval between menstruation and ovu-
lation may render gestational age calculations inaccurate,
especially for women with irregular menstrual cycles.
5
(
B
)
Finally, studies have consistently shown that the use
of the date of the last menstrual period for the purpose of
estimating gestational age is related to a greater frequency
of a later due date compared to that which is verified when
this estimate is obtained from the early ultrasound (10
to 12% versus 4%, respectively).
3,6
(
B
)
Early detection of a multiple gestation
It is known that multiple pregnancies are associated with
increased perinatal morbidity and mortality compared
to single fetus pregnancies. Therefore, early identification
of multiple pregnancies and determination of the type of
placenta play an important role in the risk stratification
and monitoring of twin pregnancies, contributing sig-
nificantly to a better prognosis. Observational studies
designed to analyze the accuracy of ultrasonography per-
formed during the first trimester in multiple pregnancies
to predict chorionicity consistently found high values of
sensitivity, specificity, positive and negative predictive
values compared to those observed from ultrasonographies
performed in the second trimester.
7,8
(
B
) Thus, ultrasound,
especially when performed by the end of week 14, is a
reliable tool for determining the number of chorions in
a twin pregnancy.
Evaluation of fetal morphology
First trimester ultrasound, performed between week 11
and week 14 of pregnancy, aims to track chromosomal
abnormalities, genetic syndromes and other fetal mal-
formations. This imaging method is well-established
for the screening of aneuploidies. In 2008, Kagan et al.
showed that the increase in cutaneous thickness pres-
ent in individuals with Down syndrome could be seen
in the first trimester (from 11 to 13 weeks plus 6 days).
They also verified that increased nuchal translucency
(thickness above the 95
th
percentile for gestational age),
when associated with maternal age and biochemical
tests such as maternal serum levels of beta-hCG free
fraction and pregnancy-associated plasma protein
(PAPP-A) provided a detection rate of 90% of cases of
trisomy 21 with a false-positive rate of 3%.
9
(
B
) Even in
the absence of chromosomal abnormality, fetuses ex-
hibiting increased nuchal translucency have an increased
risk of intrauterine death and structural abnormalities,
especially cardiac.
10
(
B
)
Some abnormalities like anencephaly are almost al-
ways detected. However, others such as myelomeningocele
or microcephaly may be difficult or impossible to iden-
tify. Numerous studies analyzing the performance of first
trimester ultrasonography to detect fetal abnormalities
found that the findings were either incidental during
screening for aneuploidy or were detected after careful
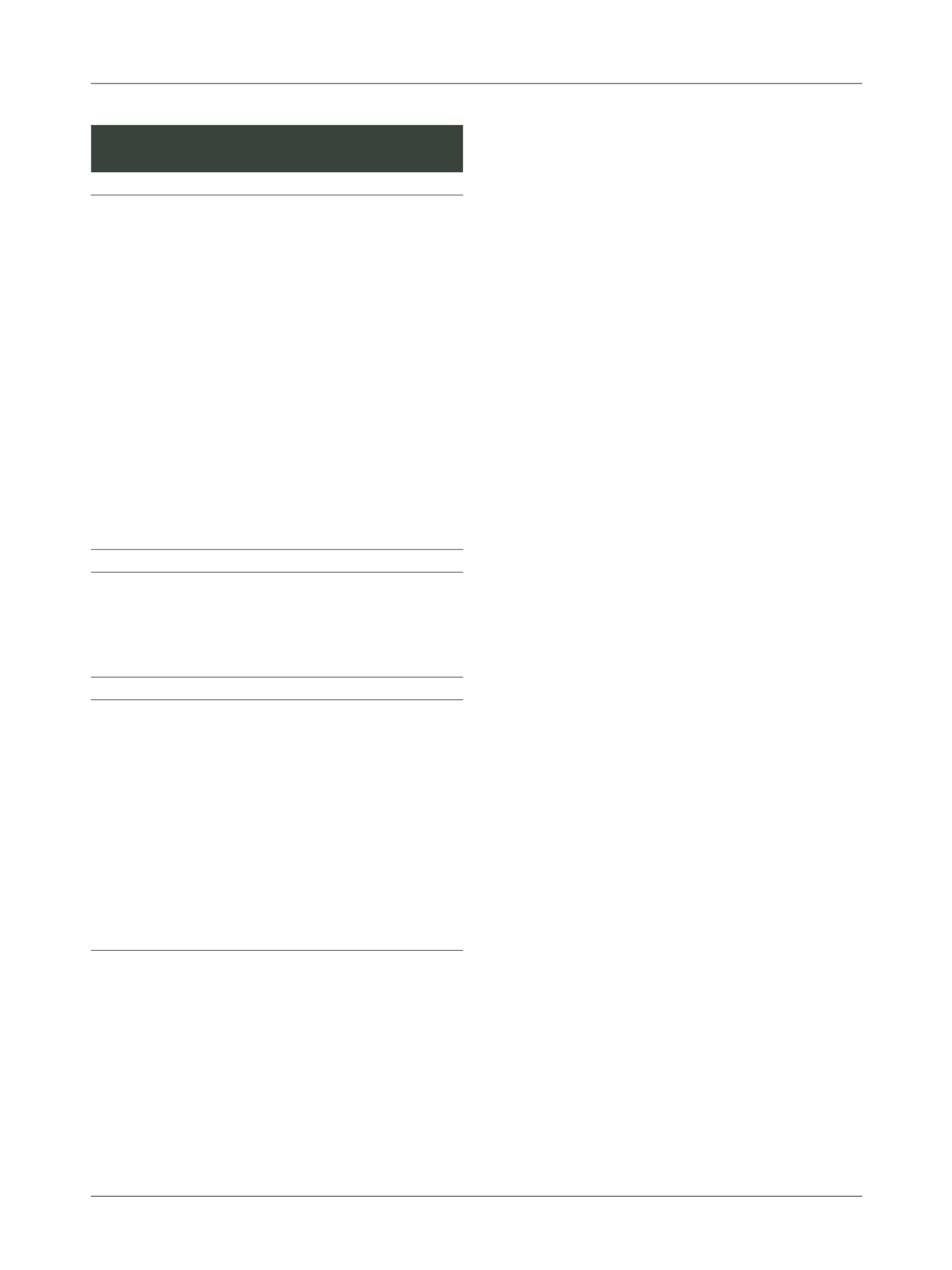
TABLE 1
Risk factors that may indicate referral to
high-risk prenatal care.
Factors related to previous conditions
Heart diseases, severe lung diseases (including bronchial asthma),
severe kidney diseases (such as chronic renal failure and transplant
patients), endocrine diseases (particularly diabetes mellitus,
hypothyroidism, and hyperthyroidism), hematological disorders
(including sickle cell disease and thalassemia), chronic hypertension
and/or patients treated with antihypertensive medication (PA >
140/90 mmHg before gestational age of 20 weeks), neurological
diseases (such as epilepsy), psychiatric disorders requiring monitoring
(psychosis, severe depression, etc.), autoimmune diseases (systemic
lupus erythematosus, other collagenoses), maternal genetic diseases,
history of deep venous thrombosis or pulmonary embolism,
gynecological disorders (uterine malformation, myomatosis, adnexal
tumors, and others), patients with infectious diseases such as
hepatitis, toxoplasmosis, HIV infection, tertiary syphilis (USG with
fetal malformation), and other STDs (condyloma), Hansen’s disease,
tuberculosis, licit or illicit drug addiction, any clinical pathology
that requires specialized monitoring.
Factors related to previous reproductive history
Intrauterine or perinatal death in previous gestation, especially if the
cause is unknown; previous history of hypertensive gestational disease
with poor obstetric and/or perinatal outcome (premature termination
of pregnancy, intrauterine fetal death, Hellp syndrome, eclampsia,
maternal ICU admission); repeated abortion; infertility.
Factors related to the current pregnancy
Restriction of intrauterine growth; polyhydramnios or oligohydramnios;
twin pregnancy; fetal malformations or fetal arrhythmia; hypertensive
disorders of gestation (pre-existing chronic hypertension, gestational
or transient hypertension); recurrent urinary tract infection or two
or more episodes of pyelonephritis; severe or unresponsive anemia
after 30-60 days of treatment with ferrous sulfate; patients with
infectious diseases such as hepatitis, toxoplasmosis, HIV infection,
tertiary syphilis (USG with fetal malformation), and other STDs
(condyloma); infections such as rubella and cytomegalovirus acquired
in the current gestation; laboratory evidence of proteinuria; gestational
diabetes mellitus; severe maternal malnutrition; morbid obesity or
low weight.
Adapted from: Ministério da Saúde, 2012.
1
















