L
eite
JF
et
al
.
186
R
ev
A
ssoc
M
ed
B
ras
2016; 62(2):184-187
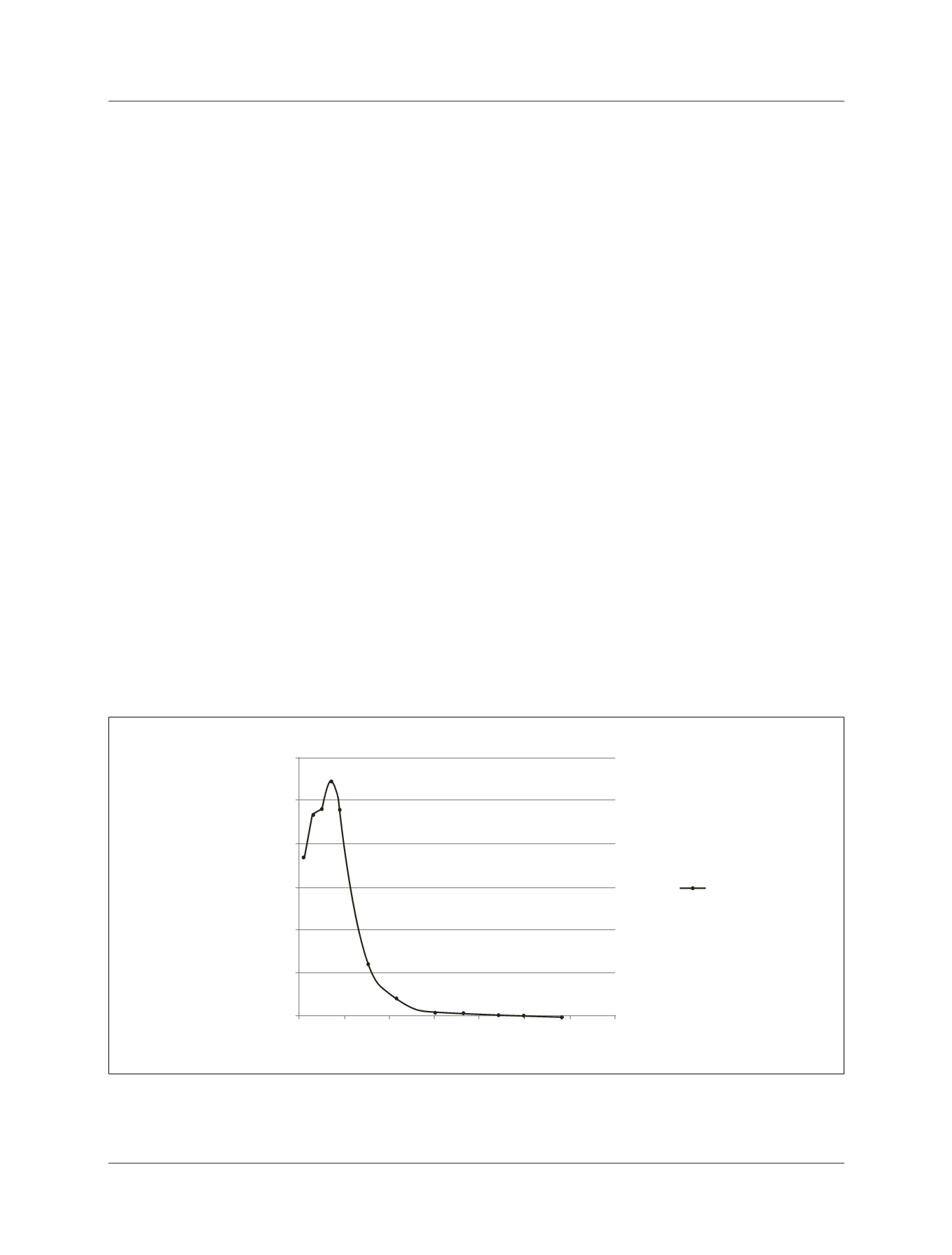
The patient was advised to continue the outpatient
follow-up where she remained in weekly monitoring, pro-
gressing with falling
β
-hCG levels. After 58 days of mon-
itoring, the
β
-hCG value was negative, as displayed in the
graph of the progression of this examination (Figure 2).
After 3 months of treatment with methotrexate, another
transvaginal ultrasound was conducted, showing the dis-
appearance of the gestational sac (Figure 3).
D
iscussion
Cesarean scar pregnancy is the rarest form of ectopic preg-
nancy. Since the first case described in 1978 until 2001,
there were only 19 cases reported. By 2006 there were 155
cases and by 2011 the number of cases described in the
literature was 751, showing a rapid increase in the inci-
dence of this type of pregnancy.
1, 8-11
The basis of the pathophysiology is the invasion of
the blastocyst in the myometrium through minimal com-
munication between the previous cesarean scar and the
endometrial cavity.
12
The cesarean scar ectopic pregnancy tends to have a
more aggressive behavior because of the risk of uterine
rupture and bleeding in the first and second trimesters
of pregnancy.
13
The risk factors are the number of prior cesarean sec-
tions, short time interval between the cesarean delivery
and the current pregnancy, and retroversion of the uter-
us which may lead to greater cesarean scar dehiscence, in-
creasing the chance of implantation of the gestational
sac in this region.
14
Transvaginal ultrasound allows early diagnosis of this
disease before tragic outcomes such as uterine rupture
or excessive bleeding and enables conservative treatment
instead of mutilating surgeries such as hysterectomy, spar-
ing fertility.
7
It also allows differential diagnosis with
abortion in progress, molar pregnancy and cervical ecto-
pic pregnancy through the ultrasound diagnostic crite-
ria proposed by Vial in 2000.
Vial et al.
7
have also proposed two types of cesarean
scar ectopic pregnancy: endogenous and exogenous. In
the endogenous type, the implementation of the gesta-
tional sac occurs in the c-section scar with the develop-
ment of the pregnancy into the uterine cavity. The exog-
enous type occurs with deeper implantation of the
gestational sac in the cesarean scar, which with the pro-
gression of the pregnancy may lead to uterine rupture
and hemorrhage in the first trimester of pregnancy.
There is still no consensus on the best mode of treat-
ment in the case of cesarean scar ectopic pregnancy. The
conduct at our service is drug treatment and outpatient
monitoring with weekly
β
-hCG exams until resolution,
only intervening surgically in the presence of heavy bleed-
ing and under these circumstances, if possible, trying to
perform uterine artery embolization prior to curettage.
15
During the outpatient follow-up, the ultrasound ex-
amination is not performed routinely, and should be re-
FIGURE 2
Graph with the progression of
b
-hCG values in the treatment of the cesarean scar ectopic pregnancy with local and systemic
methotrexate in this case report.
30,000
25,000
20,000
15,000
10,000
5,000
0
0
10
20 30 40 50
60 70
b
-hCG (mIU/)mL
7d; 27,073
9d; 23,889
1d; 18,716
23d; 1,477
15d; 6,129
30d; 479
37d; 175
44d; 84.9
51d; 21.8
58d; 2
5d; 24,070
Progression of
b
-hCG values
Values (mIU/mL)
Days (d)
3d; 23,350















