L
emes
LR
et
al
.
200
R
ev
A
ssoc
M
ed
B
ras
2016; 62(3):199-201
Pathogenesis is unknown, but the main mechanism
of accumulation of matrix components appears to be re-
lated to abnormal gene expression of extracellular pro-
tein (collagen types I and III and fibronectin) in the skin.
6
Other possible pathogenic factors would be: hyperinsu-
linemia, vascular damage, lymphatic obstruction, and
streptococcal hypersensitivity.
Systemic manifestations are rare and include: cardi-
ac, ocular, hepatosplenic, musculoskeletal and joint im-
pairment; serositis, myositis and parotiditis; as well as in-
volvement of the tongue, esophagus and pharynx.
6
On histopathological examination, the epidermis has
normal appearance and the dermis is thickened with
broad collagen bundles and mucopolysaccharide depos-
its, visualized using special staining (Alcian blue at pH
2.5 to 4.0, toluidine blue and colloidal iron). There is no
increase in the number of fibroblasts.
2
Mucin deposits
can also be evidenced in other organs such as bone mar-
row, nerves, salivary glands, and heart.
Differential diagnosis includes scleroderma and sclero-
myxedema. Scleroderma is distinguished by acral skin in-
volvement, Raynaud’s phenomenon and typical fascies
.
Histopathological examination may reveal rectified epi-
dermis, dermal sclerosis, and loss of appendages. Sclero-
myxedema, in turn, is characterized by confluent papules
which gives a hardened appearance to the skin, with wide-
spread deposition of mucin in the dermis, and fibrosis
with irregular proliferation of fibroblasts.
5,7
Several treatments have been proposed, such as topical,
systemic and intralesional corticosteroids, immunosuppres-
sives, and PUVA therapy.
1,4
Nevertheless, in most cases, the
disease is self-limiting with spontaneous resolution.
8
Its im-
portance lies in the possibility of being a systemic marker of
disease, such as difficult-to-control diabetes or paraprotein-
emias. The possibility of systemic involvement makes early
diagnosis critical for proper treatment and better prognosis.
R
esumo
Escleredema de Buschke associado a
diabetes mellitus
tipo
2 de difícil controle
Escleredema de Buschke (EB) é doença rara do tecido con-
juntivo caracterizada por endurecimento difuso e não de-
pressível da pele, principalmente nas regiões cervical, deltoi-
deanas e dorso. Enquadrado no grupo dasmucinoses cutâneas,
tem etiologia desconhecida e associação com: infecções bac-
terianas ou virais, alterações hematológicas e
diabetes mellitus
.
O exame histopatológico evidencia derme espessada comfi-
bras colágenas calibrosas separadas por fendas que corre-
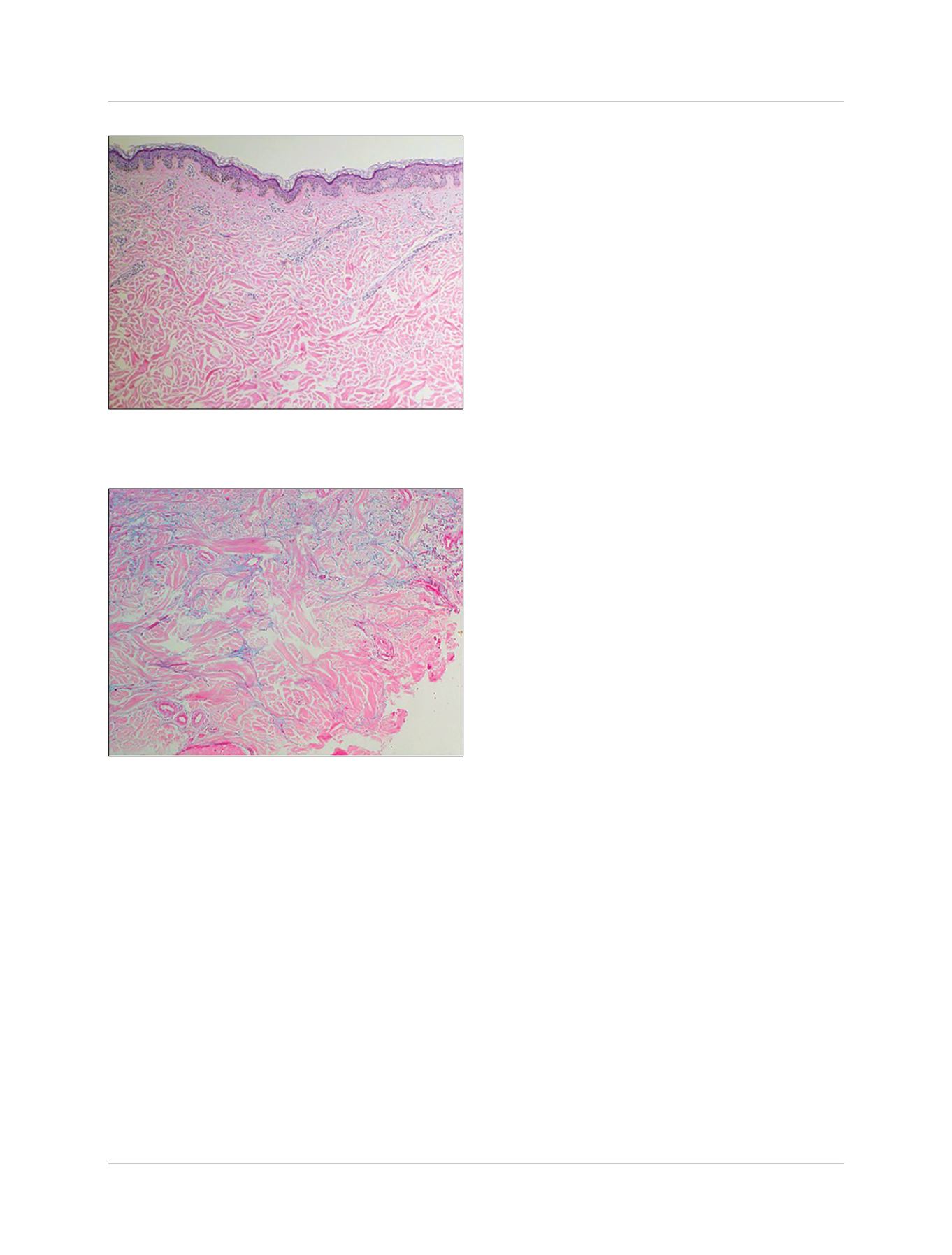
FIGURE 3
Material between thickened collagen bundles stained
with Alcian blue at pH 2.5, evidencing mucin deposits.
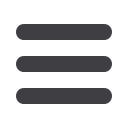
FIGURE 2
Thickened dermis, forming gaps between collagen
bundles.
influenza, measles, parotiditis, CMV and HIV. It has bet-
ter prognosis and is more prevalent in children and young
adults.
3,4
Type 2 is classically associated with paraproteinemi-
as (monoclonal gammopathy), but there are also reports
of an association with primary hyperparathyroidism, rheu-
matoid arthritis, amyloidosis and Sjogren’s syndrome. It
has a higher probability of chronic progression.
1
Type 3 SB is associated with
diabetes mellitus
(DM),
both as type 1 DM and type 2 DM. Patients most com-
monly reported in the literature are adult men with long-
standing
diabetes mellitus
with glycemic control that is dif-
ficult to achieve, obesity and high blood pressure.
Consequently, the DM has no tendency to spontaneous
resolution.
4,5















