C
ervical
cancer
:
what
’
s
new
?
R
ev
A
ssoc
M
ed
B
ras
2015; 61(6):536-542
537
tion of the specimen and thermal artifacts, which may
hinder the histological analysis, and, therefore, in such
cases scalpel conization is preferred. If there is no inter-
est in preserving fertility, the recommendation is that the
surgery should include plain hysterectomy. Bilateral sal-
pingectomy associated with hysterectomy to prevent ovar-
ian carcinoma is also recommended. However, if there is
lymphovascular invasion (very rare situation for this depth
of invasion), radical hysterectomy (Class B according to
Morrow and Querleau
6
with resection of the parametri-
um at the level of ureter) and pelvic lymphadenectomy,
or sentinel lymph node technique can be indicated. If the
patient wants to preserve fertility, radical trachelectomy
can be offered.
As for IA2 and IB1 stages, for patients who do not
want to preserve fertility, the best alternative
7
is radical
hysterectomy class C, by Morrow and Querleau, with re-
section of parametrium at the level of internal iliac artery,
which corresponds to the classical Werteim-Meigs oper-
ation, or type III-V Piver-Rutledge, in addition to pelvic
lymphadenectomy. For these stages (IA2 and IB1), the
sentinel lymph node technique can be proposed to pre-
vent radical lymphadenectomy and risks of associated
morbidities (evidence and recommendation 2B for sen-
tinel lymph node). In these stages, if the patient has a clin-
ical contraindication or if she does not accept the surgery,
the choice becomes exclusive radiotherapy, using telether-
apy supplemented by brachytherapy. Radical surgical pro-
cedures can be performed by laparotomy or laparoscopy,
including robotic surgery.
8
Surgery as initial treatment is not indicated for IB2,
IIA1 and IIA2 cancers. The probability of positive mar-
gins or other indications for radiotherapy or chemother-
apy in these stages is very high, around 80%. We know
that the addition of adjuvant therapies to surgery (chemo-
radiation) increases morbidity, worsening the quality of
life of the patient.
9-11
An important component of the treatment of cervi-
cal carcinoma in the early stages is adding radiation ther-
apy in situations at high risk for local or systemic recur-
rence. Poor prognostic indicators are obtained from
surgical specimens and include the following: positive
pelvic lymph nodes, parametrial involvement or positive
surgical margin. More recently, another category of prog-
nostic indicators was added to clinical practice and ap-
plies to patients without any of the cited criteria. These,
considered as minor criteria, are: diameter of the prima-
ry tumor associated with lymphovascular invasion, or
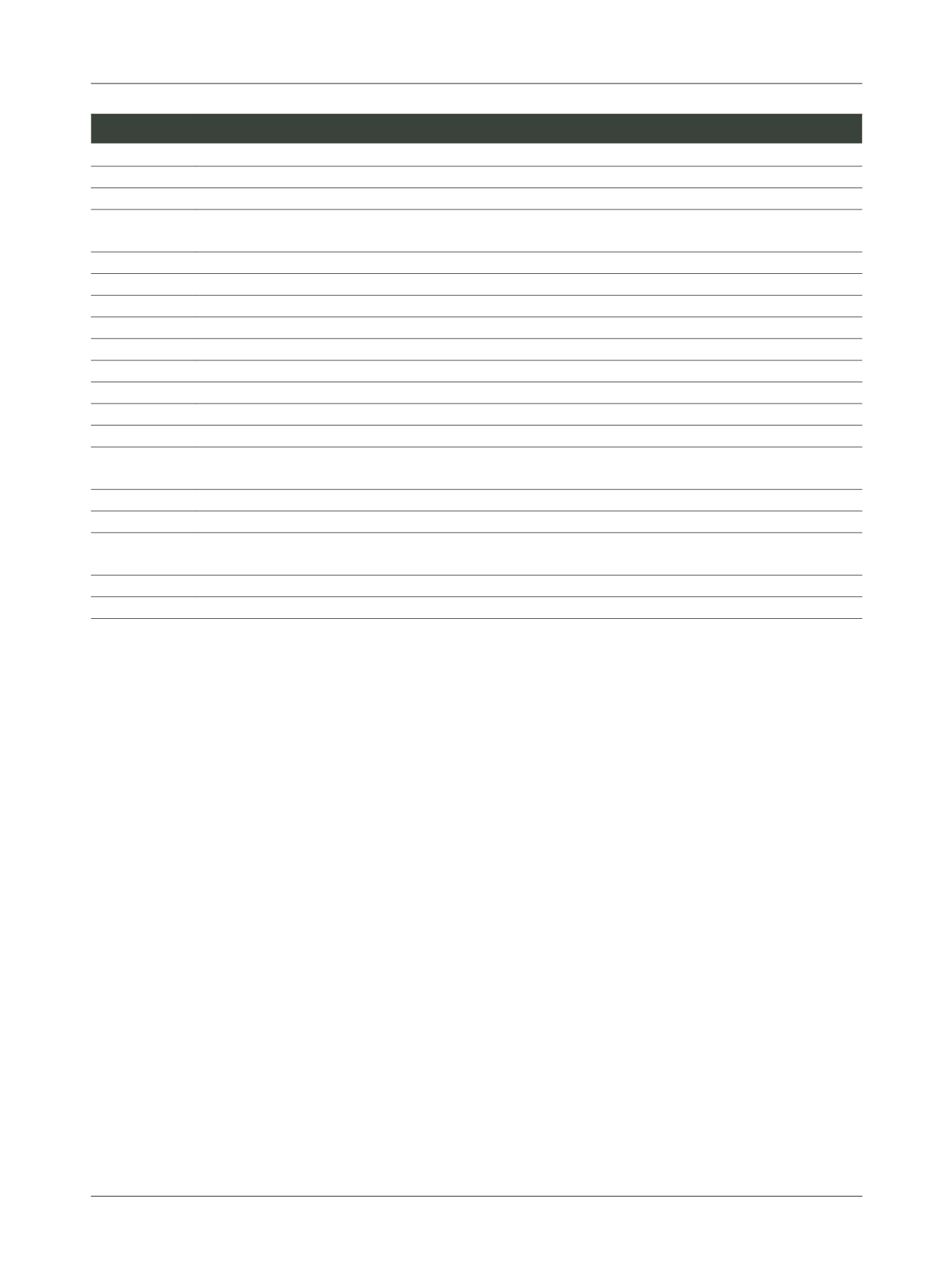
TABLE 1
Staging of cervical cancer (Figo 2009*).
Stage
Description
0
In situ
carcinoma
I
Carcinoma strictly confined to the cervix (extension to the uterine
corpus
should be disregarded)
IA
Invasive cancer identified only microscopically. Invasion is limited to measured stromal invasion with a maximum depth of
5mm and no wider than 7mm
IA1
Measured invasion of stroma ≤3mm in depth and ≤7mm width
IA2
Measured invasion of stroma >3mm and ≤5mm in depth and ≤7mm width
IB
Clinical lesions confined to the cervix, or preclinical lesions greater than stage IA
IB1
Tumor ≤4cm
IB2
Tumor >4cm
IIA
Involvement of up to the upper 2/3 of the vagina
IIA1
Tumor ≤4cm
IIA2
Tumor >4cm
IIB
Parametrial tumor involvement
III
The carcinoma has extended onto the pelvic sidewall and involves the lower third of the vagina and/or hydronephrosis and/
or non-functioning kidney
IIIA
Involvement of the lower vagina but no extension onto pelvic sidewall
IIIB
Extension onto the pelvic sidewall, or hydronephrosis/non-functioning kidney
IV
The carcinoma has extended beyond the true pelvis or has clinically involved the mucosa of the bladder and/or rectum (prov-
en by biopsy). Note: bullous edema is not considered stage IV.
IVA
Spread to bladder and/or rectum
IVB
Spread to distant organs
*Figo Proposals reviewed by the International Gynecologic Cancer Society during the Figo meeting in 2006. International Journal of Gynecology & Obstetrics. 2009;105 (2):103-194.















