D
iagnostic
accuracy
of
respiratory
diseases
in
primary
health
units
R
ev
A
ssoc
M
ed
B
ras
2014; 60(6):599-612
605
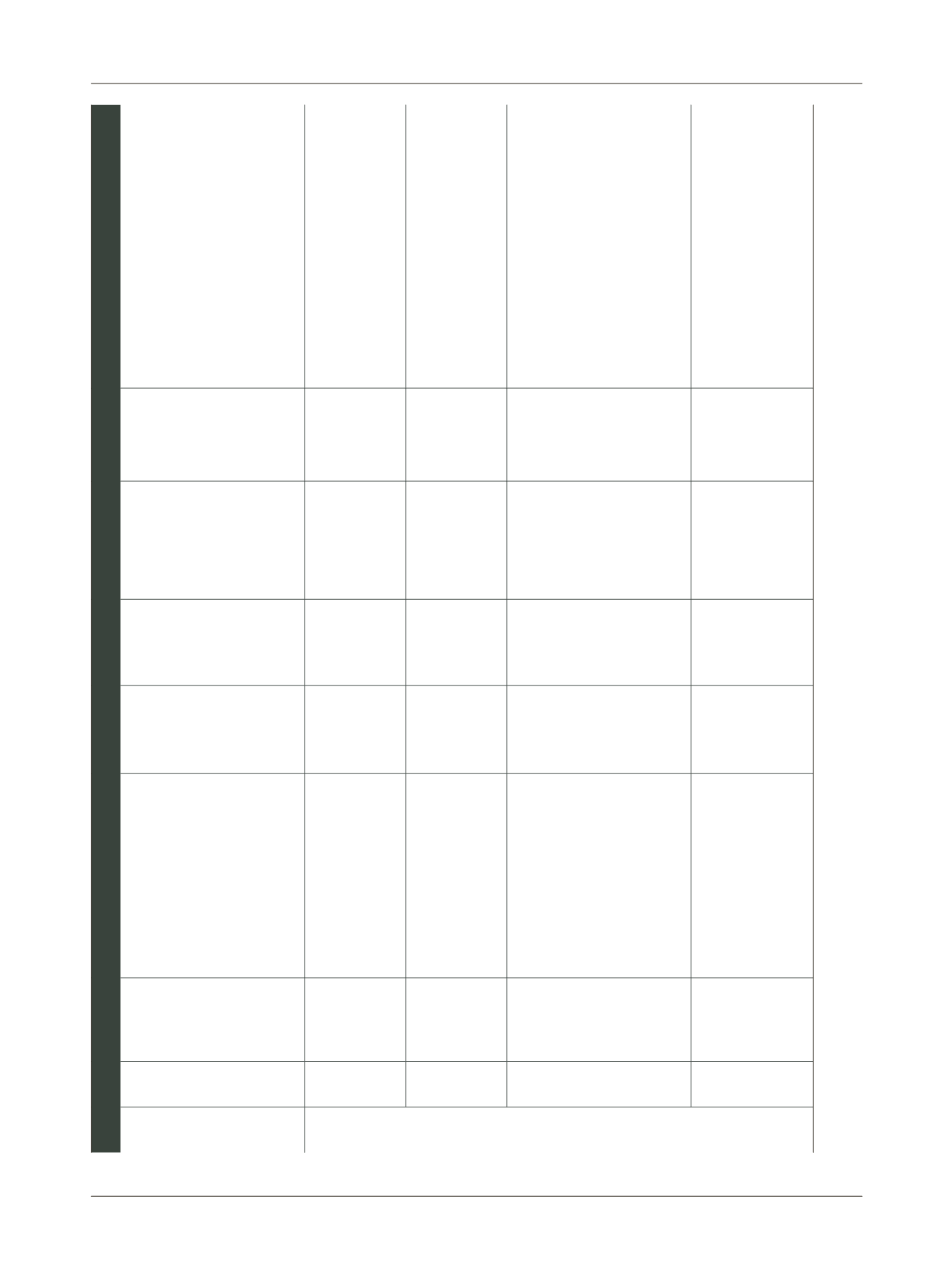
Table 1
Synopsis of the articles relating to acute respiratory tract infections (ARI), tuberculosis, asthma, COPD, and asthma and COPD in conjunction (continuation)
Asthma
22
Ward et al.,
2004, United
Kingdom
Assessed the under- and
overdiagnosis of asthma in patients
aged 16-55 years in primary care
Analysis of
questionnaire
answered by
the patients
themselves
Cross-
sectional
833 patients and
831 controls;
16-55; 34.3 average
8
The response rate was 79.1% (659/833). Among
the respondents, 60.5% (399/659) had symptoms
of bronchial hyperactivity; among those without
bronchial hyperactivity, 73.1% (190/260) were
considered asthmatic according to a review of their
medical records. The authors concluded that there
is a chance of 89.4% that patients with this
diagnosis reported in their medical records do in
fact have asthma
COPD
23
Bednarek et
al., 2008,
Poland
To investigate the prevalence and
severity of COPD in primary units
Responses to
a
questionnaire
and
spirometry
Cross-
sectional
2,250;
40-93; 56.7
2
Out of the 183 (9.3% of total) patients diagnosed
with COPD based on responses to a questionnaire
and spirometry, only 34 (18.6%) had a previous
diagnosis
24
Geijer
et al., 2005,
Netherlands
To determine the prevalence of
underdiagnosis of airflow
obstruction according to the GOLD
criteria
7
Responses to
a
questionnaire
and
spirometry
Cross-
sectional
3,985;
40- 65; 50
Not informed
Among the 702 who responded and possessed an
acceptable and reproducible spirometry, 201
(29.9%) had an obstructive pattern not previously
detected
26
Roberts et al.,
2009, United
Kingdom
To define the predictive value of
clinical diagnosis or suspicion of
COPD in primary care patients
presenting spirometric criteria for
diagnosis according to GOLD
7
Spirometry
Cross-
sectional
677; Not defined;
63.8
Not informed
Of the 503 who had clinical diagnosis and were
referred for evaluation of disease severity, 141
(28%) patients presented normal spirometry. The
remaining 302/503 (60%) had obstruction of air
flow and possible COPD according to the GOLD
criteria,
7
stage 2. The positive predictive value of
the diagnosis of COPD in primary care was 0.62 for
patients referred for severity assessment and 0.56
for patients referred for diagnostic testing
27
Zwar et al.,
2011,
Australia
Comparison of the clinical diagnosis
of COPD in primary care GPs with
spirometry
Spirometry
Cross-
sectional
1,144; 40-80; 65 56
Of the 1,144 patients identified, 445 (38.9%)
agreed to participate, undergoing spirometry. Of
these, 257 (57.8%) had spirometry consistent with
COPD; i.e., in this study, there was about 40%
overdiagnosis and many patients were treated
unnecessarily
(continues)
















