P
etribu
NCL
et
al
.
396
R
ev
A
ssoc
M
ed
B
ras
2016; 62(5):395-398
didiasis, then treated with fluconazole. Computed to-
mography of the chest showed peribronchovascular thick-
ening, areas of ground glass opacity, condensations with
air bronchograms surrounded by ground glass opacity
(halo sign) and bilateral pleural effusion (Figures 1, 2 and
3). Following guidance from the oncology team, only an-
tiretroviral therapy was maintained for immune recovery,
with subsequent evaluation regarding chemotherapy.
Two weeks after admission, the patient progressed
with disorientation, hallucinations, worsening of respira-
tory pattern, and oliguria. She had worsening of renal func-
tion, and strong metabolic acidosis. The patient was re-
ferred to the ICU, and after central venous access puncture
she progressed with respiratory failure requiring mechan-
ical ventilation. As chest X-ray showed extensive pneumo-
thorax, chest tube drainage was performed. Increased ni-
trogenous compounds and metabolic acidosis were
treated with dialysis requiring vasoactive drug due to he-
modynamic instability.
Due to the possible association of hallucinogenic symp-
toms with efavirenz and the risk of nephrotoxicity of te-
nofovir, the team chose to replace the Antiretroviral Ther-
apy (ART), introducing lopinavir/ritonavir and abacavir
with lamivudine. The antibiotic coverage was broadened
and tuberculostatic medication was started to treat a pos-
sible disseminated tuberculosis, later discarded after a neg-
ative result of PCR tests for the disease in the blood, CSF,
and urine. Cranial CT scan showed no changes, and study
of CSF ruled out any association with opportunistic dis-
eases of the central nervous system. A new CT scan of the
chest revealed consolidations at the base of both lungs
within air bronchograms and residual pneumothorax. The
patient progressed with clinical improvement, and the tra-
cheal tube was removed. Given that control chest X-ray
showed complete lung expansion, we opted for the remov-
al of the chest drain.
The patient continued with hallucinations and psy-
chomotor agitation, which were explained after psychi-
atric evaluation as sepsis-associated delirium, then treat-
ed with quetiapine.
During hemodialysis, the patient had an episode of
hypotension, followed by massive aspiration and cardio-
respiratory arrest with asystole. There was no reversal af-
ter cardiopulmonary resuscitation maneuvers.
FIGURE 3
Chest CT scan, axial mediastinal window, arterial
phase. See small bilateral pleural effusion and mediastinal lymph
nodes with preserved size.
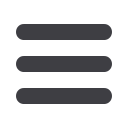
FIGURE 2
Chest CT scan, axial lung window. Some areas of
consolidation with irregular margins, and a ground glass halo giving
the appearance of flame. There is bilateral pleural effusion and
peribronchovascular infiltrate.
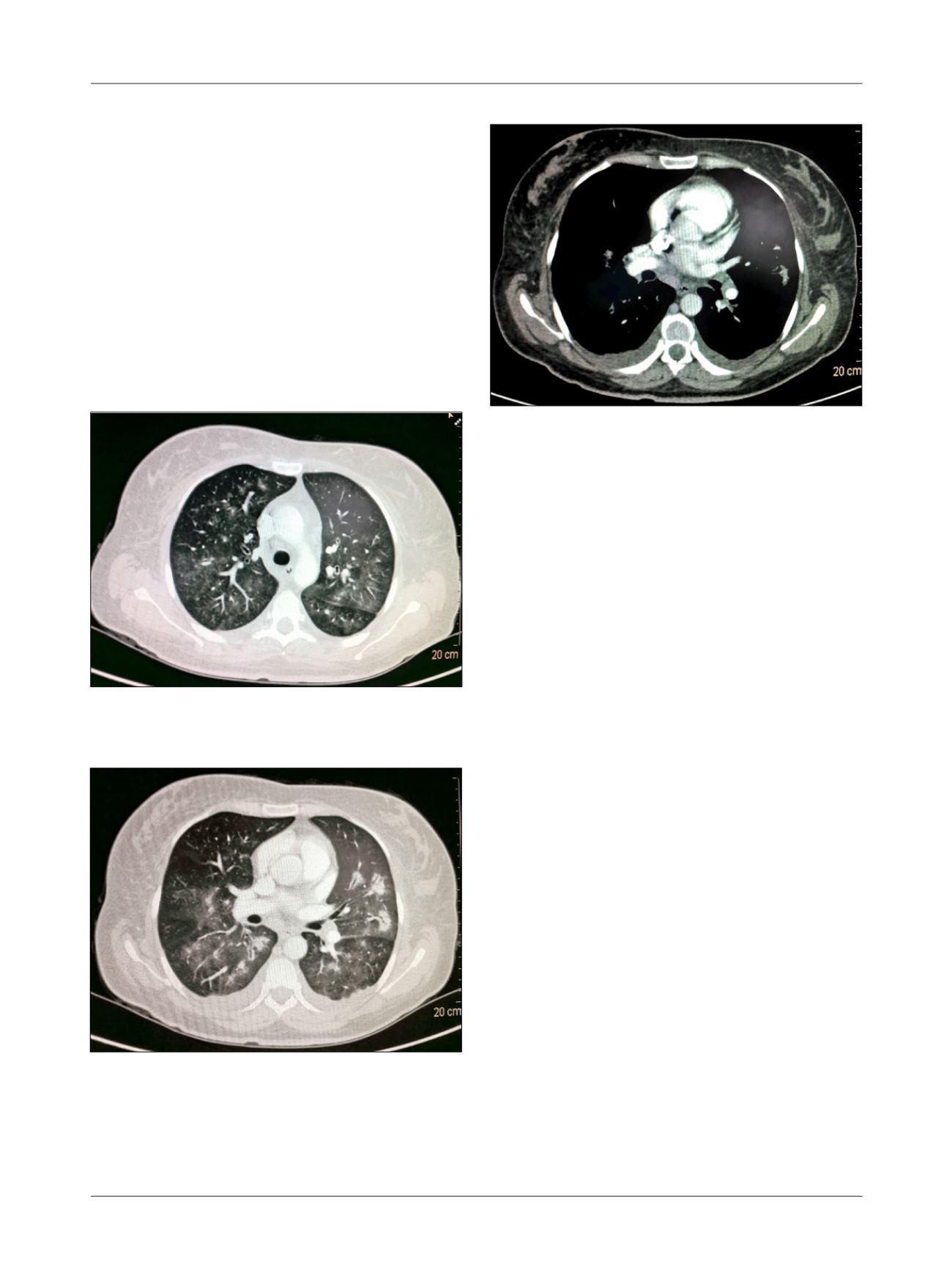
FIGURE 1
Chest CT scan, axial lung window. See areas of ground
glass opacity diffusely in both lungs.















