L
ima
FMT
de
et
al
.
390
R
ev
A
ssoc
M
ed
B
ras
2016; 62(5):389-394
The following terms were searched as “MeSH” and words
in the text:
•
•
1# (((“brain”[MeSHTerms] OR “brain”[All Fields]) AND
(“neoplasmmetastasis”[MeSHTerms] OR (“neoplasm”[All
Fields] AND “metastasis”[All Fields]) OR “neoplasm
metastasis”[All Fields] OR “metastasis”[All Fields]))
•
•
2# “brain neoplasms/secondary”[MeSH Terms] OR
“supratentorial neoplasms/secondary”[MeSH Terms]
AND ((“surgery”[Subheading] OR “surgery”[All Fields]
OR “surgical procedures, operative”[MeSH Terms] OR
(“surgical”[All Fields] AND “procedures”[All Fields]
AND “operative”[All Fields]) OR “operative surgical
procedures”[All Fields] OR “surgery”[All Fields] AND
“surgery”[All Fields]) OR “microsurgery”[MeSH Terms]
Related articles were searched from the citations in the
primary texts.
•
•
Inclusion criteria: Only randomized controlled trials
were evaluated, including those published in English,
Spanish and Portuguese.
•
•
Clinical outcomes included were: Functional indepen-
dence, survival, tumor control, cost-effectiveness, qual-
ity of life, cognitive decline and other adverse effects.
•
•
Combined results of searches: 7,963 articles were ini-
tially retrieved. 366 studies were considered clinical tri-
als, of which only three were randomized and selected
for critical evaluation of the strength of evidence. The
remaining non-randomized were excluded.
Methodological quality analysis
The three works were classified according to the Jadad
scale as ≥ 3. Considering the size of the samples in the
three studies, the one by Patchel
1
(1B)
had a strength of
91.93%, while the studies by Vecht
2
(1B)
and Mintch
3
(1B)
had the same strength, 16.96%.
The study by Patchell
1
(1B)
(1990) was randomized
at a single center, and included 48 patients to compare
surgery, followed by radiotherapy and biopsy plus radio-
therapy. Patients had mean age of 60 years; the mean Kar-
nofsky score was 90, confirming the good functional sta-
tus of patients. Randomization was done by computer
but the assessment of outcomes was not made by inde-
pendent observers or blinded to the treatment. The out-
comes studied were survival, functional independence,
tumor size progression, time to recurrence and cause of
death. Statistical analysis was performed with survival
study (Kaplan-Meier and log rank test).
The study by Vecht
2
(1B)
(1993) was a Dutch multi-
center randomized clinical trial of surgical resection, fol-
lowed by whole brain radiotherapy
versus
radiotherapy
alone. 63 patients were randomized (mean age 60 years).
Randomization was done in blocks, controlled by call
center, but outcome assessors were not blinded to treat-
ment. Assessment measures included survival, function-
ally independent survival and cause of death.
The third
3
(1B)
(Mintz, 1996) was a Canadian multi-
center study, comparing surgical resection followed by
whole brain radiotherapy
versus
whole brain radiothera-
py alone. The authors randomized 84 patients (mean age
59 years). Randomization was based on call center after
stratification for prognostic factors. Outcome assessors
were not blinded for treatment type. Outcomes included
survival (percentage), cause of death, functional status
(Karnofsky) and quality of life (using the Spitzer scale)
and surgical complications after 30 days.
Outcome data extraction
Three types of outcomes were extracted and evaluated as clus-
ters in the three randomized trials: Survival time, percentage
of lesion recurrence, and time of functional independence.
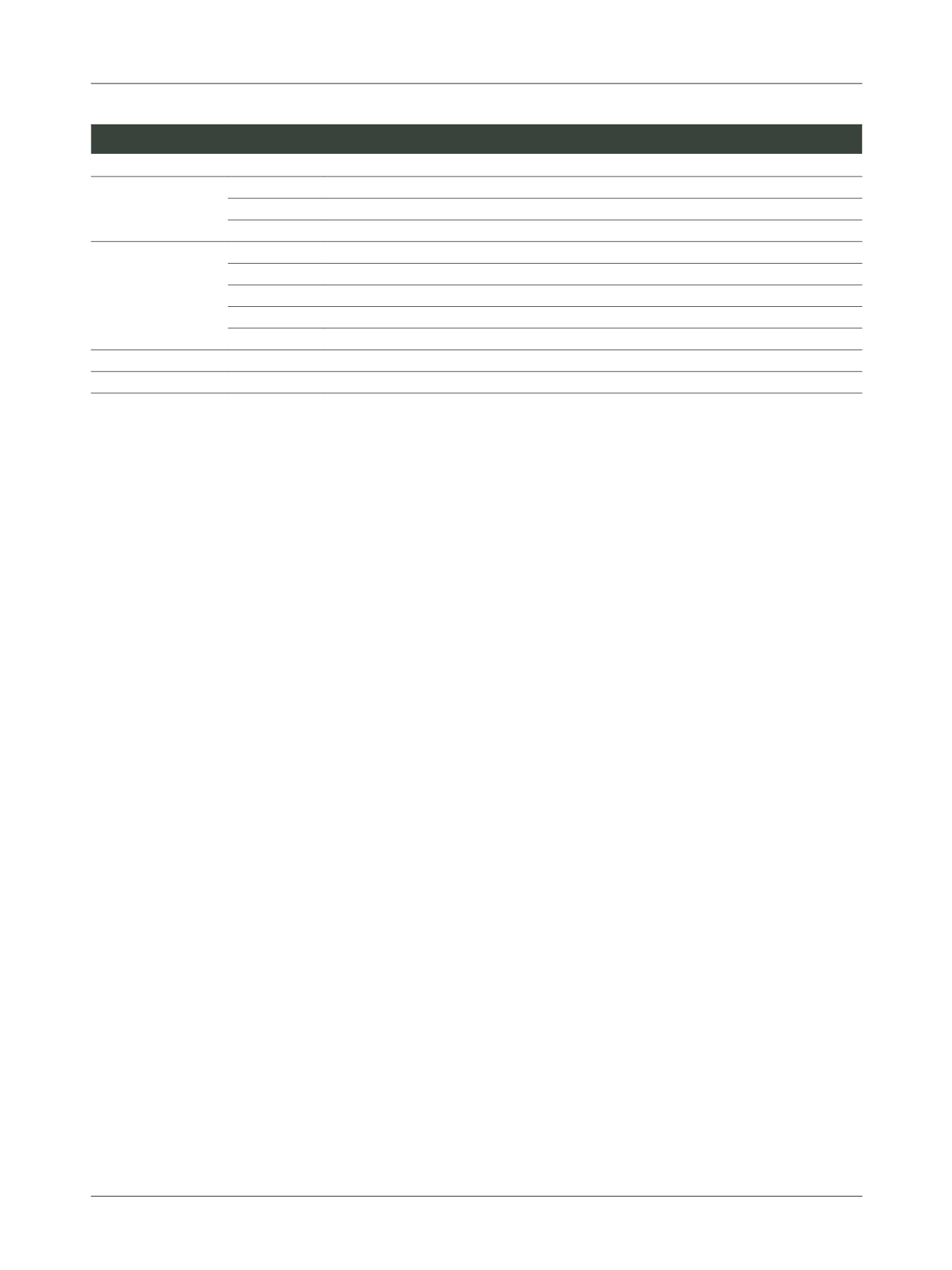
TABLE 1
Grade of recommendation and strenght of evidence.
Recommendation Evidence
Type of article
A
1A
Systematic review (with homogeneity) of randomized controlled trials
1B
Randomized controlled trials with narrow confidence interval
1C
All or none therapy outcomes
B
2A
Systematic reviews (with homogeneity) of cohort studies
2B
Cohort studies (including low-quality RCTs)
2C
Outcomes research, ecological studies
3A
Systematic review (with homogeneity) of case-control studies
3B
Case-control study
C
4
Case-reports (and poor quality cohort and case-control studies)
D
5
Expert opinion without explicit critical appraisal or first principles (physiology or animal studies)















