G
iacomazzi
CR
et
al
.
286
R
ev
A
ssoc
M
ed
B
ras
2015; 61(3):282-289
inal pelvic ultrasound, urinalysis, and blood work every
3-4 months and whole-body and brain MRIs once a year
(Table 3). This protocol was designed for subjects with
high-penetrance
TP53
mutations, such as the DNA-bind-
ing domain mutations.
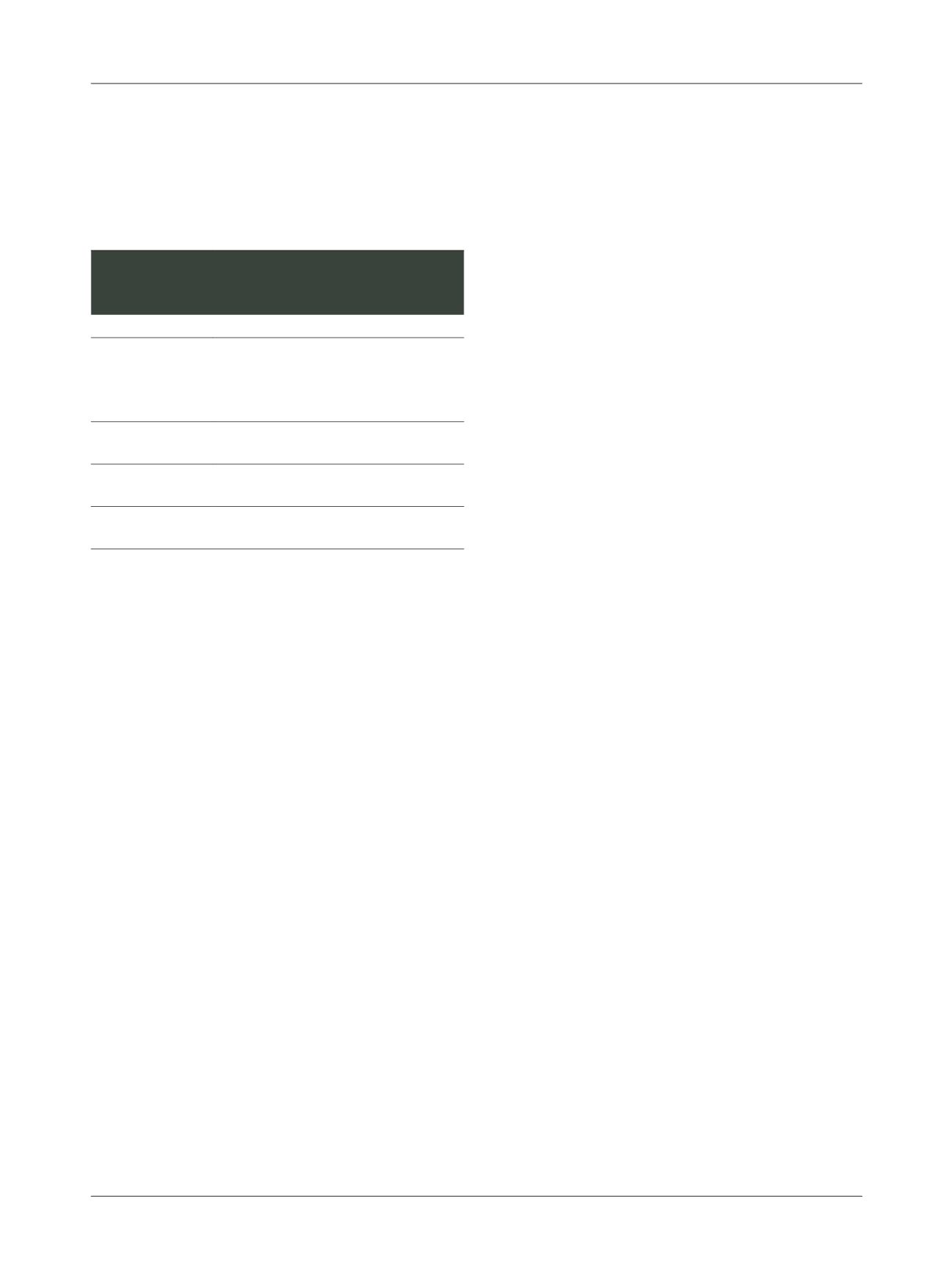
TABLE 3
Proposed screening strategy for asymptomatic
carriers of germline
TP53
mutations affecting the DNA-
binding domain.
Tumor type
Screening strategy
Adrenocortical
carcinoma
Abdominal ultrasound every 4 months
Urinalysis every 4 months
b
-hCG, AFP, 17OHP, testosterone, DHEAS,
androstenedione, ESR, LDH every 4 months
Central nervous
system tumors
Whole-body MRI once yearly
Bone and soft tissue
sarcomas
Whole-body MRI once yearly
Leukemia and
lymphoma
Complete blood count every 4 months
17OHP: 17-hydroxyprogesterone;
AFP:
α
-fetoprotein;
b
-hCG: beta-human chorionic gonadotropin;
DHEAS: dehydroepiandrosterone sulfate;
ESR: erythrocyte sedimentation rate;
LDH: lactate dehydrogenase;
MRI: magnetic resonance imaging.
Source: Villani et al. 2011.
40
Psychological aspects
Pre-symptomatic genetic testing of children and adoles-
cents is indicated whenever preventive interventions that
require initiation before adulthood are available.
43
One
of the concerns of predictive testing in cancer genetics,
especially among children, are potential psychological
adverse events.
Currently, the psychological effects of intensive can-
cer screening in
TP53
mutation carriers are not clear. How-
ever, results from preliminary studies are encouraging
and report psychological benefits from adherence to in-
tensive screening practices in LFS families.
44,45
The risks
and benefits both of revealing and of withholding a clin-
ical or molecular diagnosis of cancer predisposition have
been the subject of extensive debate in the literature.
46-48
Psychological harm may be involved in issues such as in-
creased worry about cancer risk, the need for periodic lab-
oratory and imaging tests and the anxiety that precedes
and follows them, and the burden of testing itself. Some
studies have found that a passive, pessimistic coping style,
low social aspirations, and precarious social support net-
works also have a negative impact on mutation carriers,
as does negative perception of the disease and the risk of
cancer itself.
49
However, during counseling of at-risk chil-
dren, these psychological vulnerabilities can be identified
before any diagnostic or therapeutic measures are taken,
thus enabling prevention and mitigation of adverse psy-
chological reactions.
50
Whenever possible, predictive genetic testing should
be performed when the child has a bare minimum of ma-
turity and understanding as to the nature of decision-mak-
ing and its implications. In other words, as children’s in-
tellectual and psychosocial skills mature, they become
increasingly capable of communicating and taking part in
decisions that affect them.
43
Most authors believe that pre-
dictive genetic counseling and follow-up of minors is jus-
tified by the high risk of cancer in LFS/LFL and by the prov-
en benefits of intensive screening.
17,42
When predictive
diagnosis is justified in children who are not mature
enough to take part in the decision-making process, the
child’s parents must be supported throughout the testing
process and also later on, when information regarding can-
cer risk is disclosed to the carrier child or adolescent. The
literature has shown that adolescents and young adults
usually regard genetic counseling as an opportunity to
know the risks of hereditary cancer and support decision-
-making on aspects such as marrying and having children.
51
Several studies show that families with LFS/LFL tend to
trust and comply with genetic counseling, as they feel saf-
er when educated on the disease and able to understand
the diagnosis and better cope with its outcome.
43,50
Genetic counseling of LFS/LFL and bioethical aspects
Genetic counseling for hereditary conditions is an edu-
cational activity that enables the exchange of informa-
tion between professionals and patients (and, as neces-
sary, their relatives). When properly informed, patients
and their relatives are empowered to make better deci-
sions.
52
Decision-making capacity is also related to indi-
vidual psychological and moral development and to is-
sues of voluntariness. The patient’s affective relationships
and personal system of values and beliefs are key elements
in this process.
53
From the patient’s standpoint, at least four factors
must be taken into account during genetic counseling:
the availability of choices; potential cognitive biases in
the presentation of these choices; embedding of a partic-
ular decision within a broader moral framework, such as
the patient’s involvement with other family members;
and the patient’s own concerns.
3,54
One bioethics issue is at the core of genetic counsel-
ing: conflict between the moral duties of warning family
members of genetic risk
versus
the patient’s right not to















