C
all
for
aWarEnESS
of
thE
uPDatED
DiagnoStiC
CritEria
anD
CliniCal
managEmEnt
for
PatiEntS
With
tuBErouS
SClEroSiS
ComPlEx
r
Ev
a
SSoC
m
ED
B
raS
2014; 60(2):94-96
95
no longer independent features due to their low speci-
icity for TSC (Table 1).
1
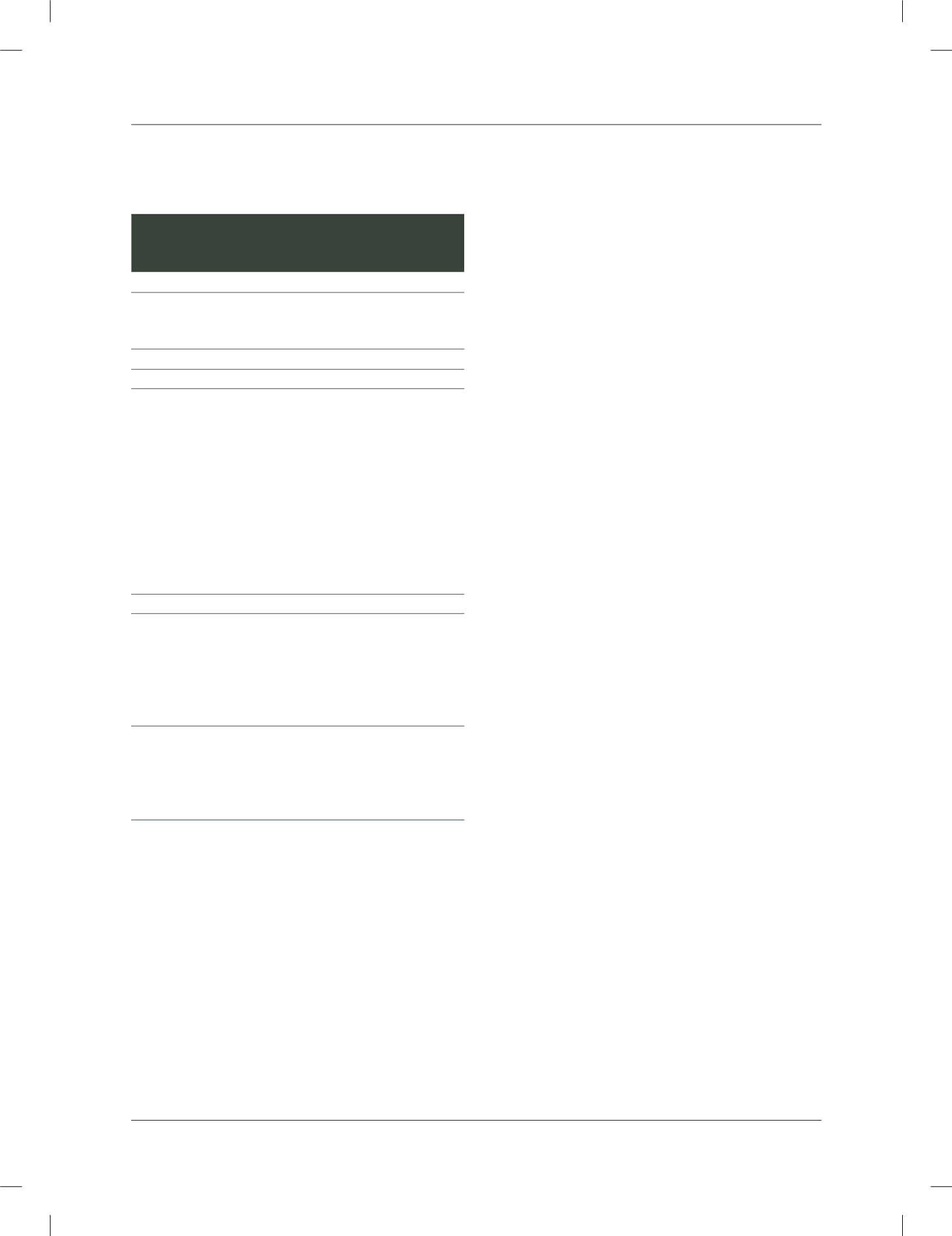
TABLE 1
Revised Criteria for Tuberous Sclerosis Complex
Diagnosis according to the 2012 International Tuberous
Sclerosis Complex Consensus Conference
1
A. Genetic diagnostic criteria
The identification of either a TSC1 or TSC2 pathogenic mutation in
DNA from normal tissue is sufficient to make a definite diagnosis of
tuberous sclerosis complex (TSC)
a
.
B. Clinical diagnostic criteria
Major features
1. Hypomelanotic macules (>3, at least 5 mm in diameter)
2. Angiofibromas (>3) or cephalic fibrotic plaque (face or scalp)
3. Nail fibromas (>2)
4. Shagreen patch
5. Multiple retinal hamartomas
6. Cortical dysplasias
b
7. Subependymal nodules
8. Subependymal giant cell astrocytomas
9. Cardiac rhabdomyoma
10. Lymphangioleiomyomatosis (LAM)
c
11. Angiomyolipoma (>2)
c
Minor features
1. Confetti skin lesions
2. Pits in dental enamel (>3)
3. Intraoral fibromas (>2)
4. Localized retinal achromia
5. Multiple kidney cysts
6. Nonrenal hamartomas
Definite diagnosis:
Two major features or one major feature with two or more minor
features.
Possible diagnosis:
Either one major feature or two or more minor features.
a
A pathogenic mutation is defined as a mutation that clearly inactivates the function of the
TSC1 or TSC2 proteins, prevents protein synthesis or is a missense mutation whose effect on
protein function has been established by functional assessment
(www.lovd.nl/TSC1,
www.lovd/TSC2).
b
Cortical dysplasia includes tubers and cerebral white matter radial migration lines.
c
A combination of the two major clinical features (LAM and angiomyolipomas) without other
features does not meet criteria for a definite diagnosis.
Besides the review of the clinical diagnosis of TSC, the
2012 panels included its genetic deinite diagnosis (Ta-
ble 1). Nearly 75 to 90% of TSC patients tested by con-
ventional molecular methods have a mutation detected
in
TSC1
or
TSC2
gene. Therefore, although the lack of
mutation identiied does not exclude TSC, the inding of
one pathogenic mutation in
TSC1
or
TSC2
in normal tis-
sue is at present suficient for the diagnosis. This may be
particularly important for young patients with inconclu-
sive clinical diagnosis who may beneit from early and
thorough surveillance of recognized or for novel lesions.
By pathogenic mutation it is understood those that im-
pact on protein synthesis or function, such as large ge-
nomic deletions; the ones that cause shift in the reading
frame for aminoacids; the change of a codon into a stop
codon, causing truncated protein; or a missense muta-
tion switching aminoacids. The latter needs experimen-
tal functional validation to be considered pathogenic.
Any other
TSC1
or
TSC2
variant whose effect on the pro-
tein is uncertain does not meet that criterium.
1
It is not our goal to summarize here the speciic gui-
delines for surveillance and treatment for lesions in each
different organ. Those have been widely explained by
Krueger
et al
(2013). Based on the data available, the 2012
Consensus group has determined four categories of re-
commendation which have been applied to each aspect
evaluated. The recommendation categories were based
on the literature study level of evidence and the appro-
priateness of the diagnostic or therapeutic intervention:
•
Category 1: Based upon high-level evidence, there
is uniform consensus that the intervention is ap-
propriate;
•
Category 2A: Based upon lower-level evidence, the-
re is uniform consensus that the intervention is ap-
propriate;
•
Category 2B: Based upon lower-level evidence, the-
re is consensus that the intervention is appropria-
te;
•
Category 3: Based upon any level of evidence, a con-
sensus on appropriate intervention cannot be rea-
ched.
Methods and periodicity for surveillance have been des-
cribed.
2
The indings that the proteins expressed by the
TSC1
and
TSC2
genes as a heterodimer have inhibitory roles on
the mammalian target of rapamycin (mTOR) led to cli-
nical trials of rapamycin or analogs (mTOR inhibitors)
to treat subependymal gyant cell astrocytoma (SEGA),
angiomyolipoma and lung lymphangioleiomyomatosis
(LAM). In different countries, regulatory agencies have
approved the indication of mTOR inhibitors for distinct
TSC lesions. Clinical indications for mTOR inhibition
therapy have been reviewed by the consensus group. Cli-
nical conditions that may beneit from short-termmTOR
inhibition drugs are: growing, asymptomatic SEGA;
asymptomatic, growing, angiomyolipomas larger than 3
SCIELO BOOK.indb 95
4/22/14 4:35 PM















