H
ospitalization
due
to
exacerbation
of
COPD: “R
eal
-
life
”
outcomes
R
ev
A
ssoc
M
ed
B
ras
2017; 63(6):543-549
547
Table 1 shows that patients have a high average age
and that in some the follow-up period with a pulmonolo-
gist was only 6 months, that is, the diagnosis was recent,
and as a consequence, the number of spirometries per-
formed was small. It is interesting to note that several
patients (38) were not included in the study because they
had never undergone spirometry (inclusion criteria), a
fundamental exam for the diagnosis of COPD.
18
COPD
underdiagnosis results in late recognition of the disease
and in later stages.
19,20
Early detection of airflow limitation
and smoking cessation intervention may delay the decline
of lung function, reduce COPD symptoms, and improve
the patient’s quality of life.
In a retrospective study of COPD patients hospital-
ized for respiratory failure over a period of 8 years, only
31% had a diagnosis confirmed by spirometry despite
having a clinical diagnosis of eCOPD,
19
which character-
izes overdiagnosis.
Patients with a smoking load ≥ 10 packs/year were
included in this study. Smoking is the most frequent
cause of COPD, although there are other risk factors such
as exposure to occupational dust, air pollution and bio-
mass burning.
20
We observed that 42% of our patients
reported exposure to wood stoves.
Still in relation to the characteristics of the sample,
17% of the patients had a history of bronchitis in childhood.
It is known that the prevalence of asthmatics who smoke
is similar to that of the general population, and that many
COPD patients may present a history of asthma prior to
COPD. COPD is often confused with asthma.
21,22
The co-
existence of these conditions is called asma-COPD overlap
syndrome.
23
With increasing age, there is an increase in the
proportion of patients with this syndrome. Some studies
found that 55% of COPD patients over 50 years of age had
asthma, whereas in other studies the prevalence of asthma-
‑COPD overlap syndrome ranged from 13 to 19%.
23
Patients hospitalized with eCOPD had 4.2±2.2 comor-
bidities, which is consistent with reports in the medical
literature that these are more frequent in patients with
COPD than in the general population.
24
Some comor-
bidities present in patients with COPD affect the progno-
sis, as described by Divo and Cote.
6
In our study, the Cote
score was higher than 4 for ten patients (21%), whichmeans
an increased risk of death. There is evidence that the spe-
cific management of COPD reduces the number of exac-
erbations leading to clinical stability for comorbidities with
reduced mortality. The same happens with the treatment
of comorbidities, which affects the stability of COPD.
24,25
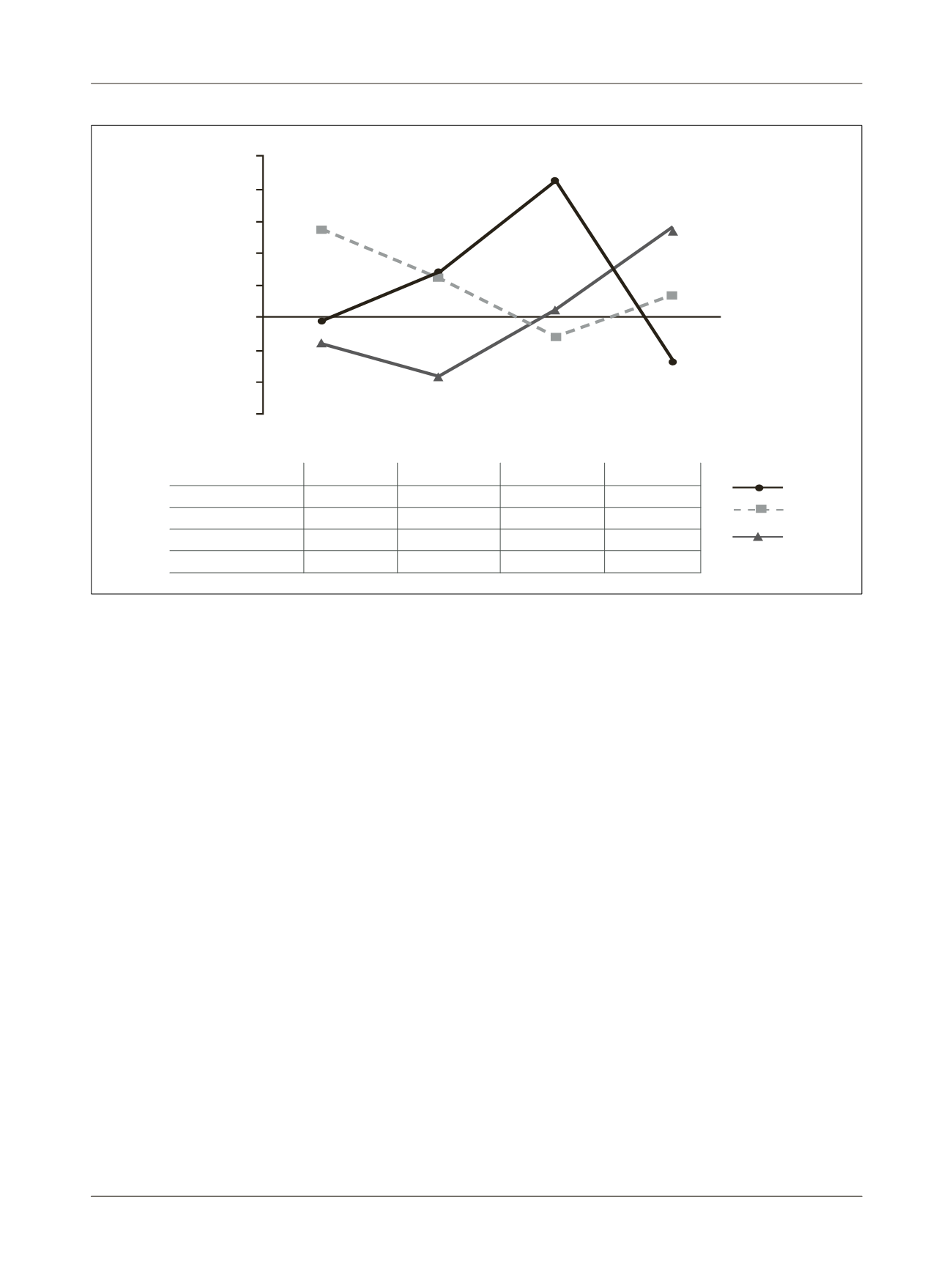
FIGURE 2
Standardized variables related to disease severity (age, CAT, FEV
1
and BMI) allowed grouping of patients into three clusters.
Age (years) CAT (total)
BMI (kg/m
2
) FEV
1
pre (L)
Cluster 1 (n=8)
73±3
26±5
37±8
0.94±0.28
Cluster 2 (n=14)
77±7
22±7
23±4
0.85±0.24
Cluster 3 (n=23)
69±6
18±6
26±3
1.45±0.40
p(<0.05)
0.003
0.035
<0.001
<0.001
Z score
5,0
4,0
3,0
2,0
1,0
0,0
-1,0
-2,0
-3,0
















