
H
anna
and
P
imentel
294
R
ev
A
ssoc
M
ed
B
ras
2017; 63(4):293-298
•
•
Low risk: PSA ≤ 10 ng/mL plus Gleason ≤ 6 and stage
T ≤ 2a disease.
•
•
Moderate risk: one of the criteria above is not met.
•
•
High risk: two of the criteria above not met, or Glea-
son > 7 or T > 2b or PSA > 20 ng/mL.
In early tumors, radical locoregional treatment can alter the
natural course of the disease by decreasing local progression,
distant metastasis and death from prostate cancer.
10-12
The ideal therapy for localized prostate cancer is still
the subject of controversy. The long natural history of
early and low-risk tumors means that not all patients
need treatment if their life expectancy is less than 10 years
(active surveillance
13
).
Several treatment alternatives may be employed in
initial management as monotherapy or combination
therapy, such as radical prostatectomy, external beam RT
and brachytherapy (BT). However, there is still no direct
comparison between the three modalities based on ran-
domized clinical trials.
BT has been used in prostate cancer since the last
century. However, in the 1980s, there were incorporations
to the historically described technique that made it more
systematized, such as the use of real-time images to guide
the placement of isotopes, computerized planning and, last-
ly, the transperineal approach – less invasive and less toxic.
In fact, in comparison to other modalities, BT became
attractive for some reasons: a supposed lower invasiveness
and toxicity compared to surgery and even to external ir-
radiation; it allows the patient to return to normal activities
faster; and, finally, it is a treatment that generates less cost.
14
Below, practical questions to be answered in this
guideline will be presented. BT (also called an implant)
can be divided into two modalities:
•
•
High-dose rate brachytherapy (HDR-BT): use of iridi-
um-192 as a high activity source, controlled by a re-
mote system that connects several needles placed stra-
tegically in the prostate and is later removed from the
patient (temporary implantation).
•
•
Low dose-rate brachytherapy (LDR-BT): insertion of
seeds of iodine-125 (I-125) or palladium-103 (Pd-103)
into needles that will be strategically implanted into
the prostate and will remain in position allowing the
release of the irradiating dose (seed implantation).
The modalities are similar in terms of complexity, and
usually follow the steps below:
•
•
Pre-implantation preparation (low-residue diet, intes-
tinal preparation, pre-anesthetic visit, etc.).
•
•
Anesthesia.
•
•
Preplanning (placing the patient in a position favor-
able to implantation and acquisition of ultrasound
images to determine the strategy of insertion of the ra-
dioactive material), also called volume study.
•
•
Medical and physical planning.
•
•
The implantation itself: refers to the insertion of the
BT needles, guided by a template (installed in a device
called stepper unit or attached to the patient’s perine-
um using sutures and stitches on the skin) and ultra-
sound (fluoroscopy can also be used, if available).
•
•
Cystoscopy for urinary tract inventory, if available.
•
•
Post-implant dosimetry (CT scan to check the posi-
tion of the radioactive material) – performed only in
low dose-rate BT.
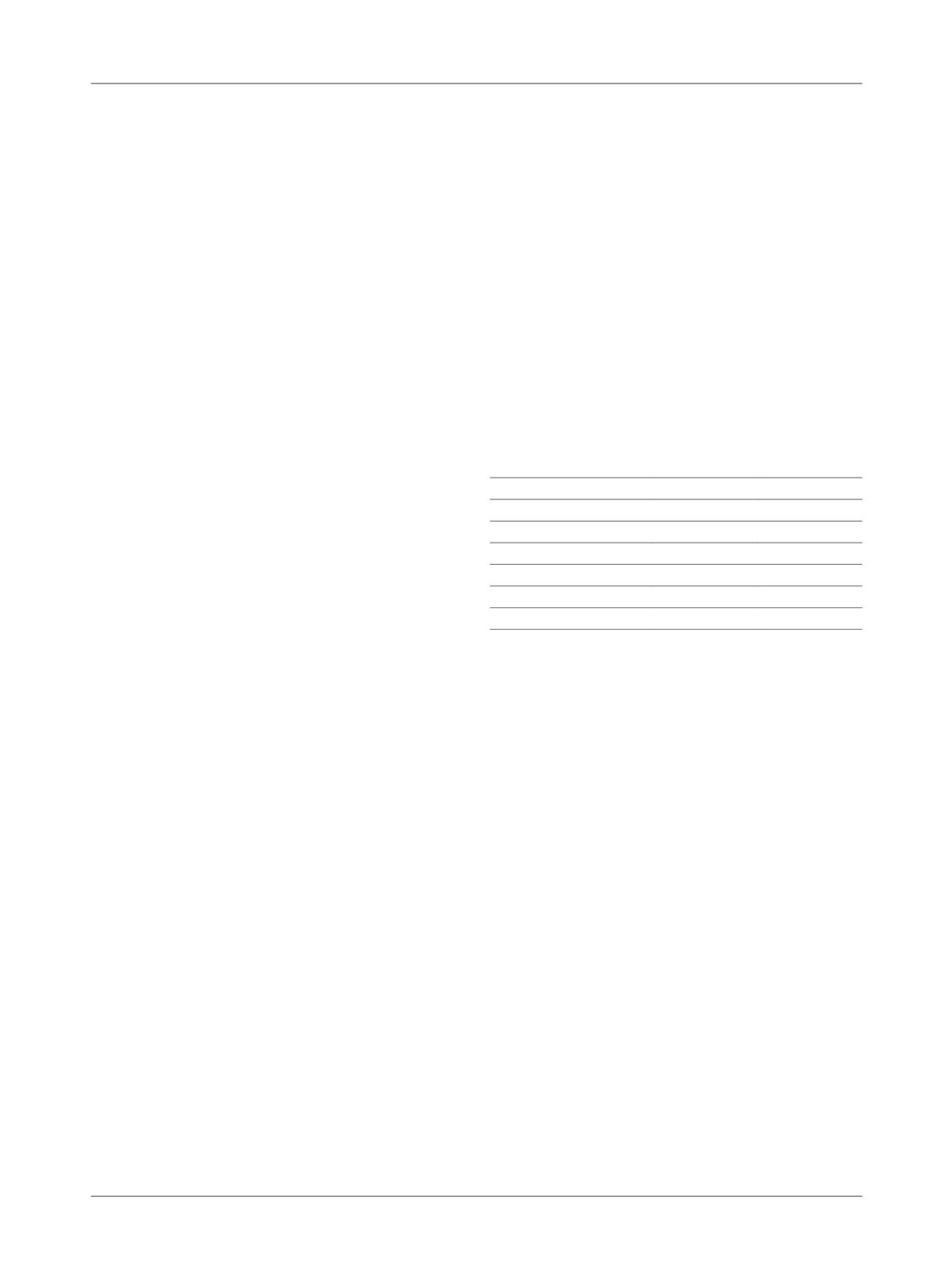
High dose-rate Low dose-rate
Implant type
Temporary
Permanent
Anesthesia
Yes
Yes
Pre-planning
Yes
Yes
Outpatient
Yes
No
Number of procedures
More than one One
Conference in real time
Yes
Yes
Post-implant dosimetry
No
Yes
Pre-procedure preparation Yes
Yes
I
s
low
dose
-
rate
brachytherapy
an
equally
effective
option
as monotherapy
?
For low-risk patients, there are two randomized studies
comparing BT and surgery as monotherapy of patients
with localized tumors.
A North American and Canadian multicenter study
15
included 263 patients with localized prostate tumors and
compared radical prostatectomy with LDR-BT (144 Gy).
At 5.3 years of median follow-up, PSA levels reached by
the two groups were 0.05 ng/mL and 0.05 ng/mL, dem-
onstrating equivalent biochemical control
(A)
.
A similar study performed by Italian centers
16
in-
cluded 200 patients with low risk tumors and median age
of 65 years. After 5 years of follow-up, 174 of them could
be analyzed. Biochemical failure-free survival rates were
at 91% in the surgery group and 91.7% in the LDR-BT
group, which did not reach statistical significance
(A)
.
Comparison between BT monotherapy and external
beam RT is the object of some observational studies. An
American series of case reports
17
included 282 patients
with low-risk tumors (137 treated with BT and 145 treat-
ed with external beam RT). After 5 years of follow-up,
there were 8% of relapses in each group (p=0.09), with a
similar toxicity profile
(C)
.
















